- Record: found
- Abstract: found
- Article: found
Serum GFAP for stroke diagnosis in regions with limited access to brain imaging (BE FAST India)
Read this article at
Abstract
Introduction
Despite a high burden of stroke, access to rapid brain imaging is limited in many middle- and low-income countries. Previous studies have described the astroglial protein GFAP (glial fibrillary acidic protein) as a biomarker of intracerebral hemorrhage. The aim of this study was to test the diagnostic accuracy of GFAP for ruling out intracranial hemorrhage in a prospective cohort of Indian stroke patients.
Patients and methods
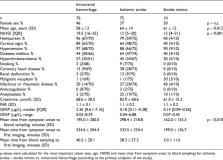
This study was conducted in an Indian tertiary hospital (Christian Medical College, Ludhiana). Patients with symptoms suggestive of acute stroke admitted within 12 h of symptom onset were enrolled. Blood samples were collected at hospital admission. Single Molecule Array technology was used for determining serum GFAP concentrations.
Results
A total number of 155 patients were included (70 intracranial hemorrhage, 75 ischemic stroke, 10 stroke mimics). GFAP serum concentrations were elevated in intracranial hemorrhage patients compared to ischemic stroke patients [median (interquartile range) 2.36 µg/L (0.61–7.16) vs. 0.18 µg/L (0.11–0.38), p < 0.001]. Stroke mimics patients had a median GFAP serum level of 0.14 µg/L (0.09–0.26). GFAP values below the cut-off of 0.33 µg/L (area under the curve 0.871) ruled out intracranial hemorrhage with a negative predictive value of 89.7%, (at a sensitivity for detecting intracranial hemorrhage of 90.0%).
Related collections
Most cited references36
- Record: found
- Abstract: not found
- Article: not found
2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol
- Record: found
- Abstract: found
- Article: not found
Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review.
- Record: found
- Abstract: found
- Article: not found