- Record: found
- Abstract: found
- Article: found
Area Socioeconomic Status is Associated with Refusal of Recommended Surgery in Patients with Metastatic Bone and Joint Disease
Read this article at
Abstract
Background
This study sought to identify associations between the Yost Index, a geocoded area neighborhood socioeconomic status (nSES) score, and race/ethnicity with patient refusal of recommended surgery for metastatic bone disease.
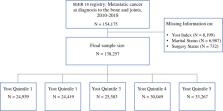
Methods
Patients with metastatic bone disease were extracted from the Surveillance, Epidemiology, and End Results database. The Yost Index was geocoded using factor analysis and categorized into quintiles using census tract-level American Community Service (ACS) 5-year estimates and seven nSES measures. Multivariable logistic regression models calculated odds ratios (ORs) of refusal of recommended surgery and 95% confidence intervals (CIs), adjusting for clinical covariates.
Results
A total of 138,257 patients were included, of which 14,943 (10.8%) were recommended for surgical resection. Patients in the lowest nSES quintile had 57% higher odds of refusing surgical treatment than those in the highest quintile (aOR = 1.57, 95% CI 1.30–1.91, p < 0.001). Patients in the lowest nSES quintile also had a 31.2% higher age-adjusted incidence rate of not being recommended for surgery compared with those in the highest quintile (186.4 vs. 142.1 per 1 million, p < 0.001). Black patients had 34% higher odds of refusing treatment compared with White patients (aOR = 1.34, 95% CI 1.14–1.58, p = 0.003). Advanced age, unmarried status, and patients with aggressive cancer subtypes were associated with higher odds of refusing surgery ( p < 0.001).
Conclusions
nSES and race/ethnicity are independent predictors of a patient refusing surgery for metastatic cancer to bone, even after adjusting for various clinical covariates. Effective strategies for addressing these inequalities and improving the access and quality of care of patients with a lower nSES and minority backgrounds are needed.
Related collections
Most cited references79
- Record: found
- Abstract: found
- Article: not found
Clinical features of metastatic bone disease and risk of skeletal morbidity.
- Record: found
- Abstract: found
- Article: not found
Cancer Disparities by Race/Ethnicity and Socioeconomic Status
- Record: found
- Abstract: found
- Article: not found