- Record: found
- Abstract: found
- Article: found
Effect of MAFLD on albuminuria and the interaction between MAFLD and diabetes on albuminuria

Read this article at
Abstract
Objective
To investigate the effects of metabolic associated fatty liver disease (MAFLD) on chronic kidney disease (CKD) and abnormal albuminuria and the interaction between MAFLD and diabetes on abnormal albuminuria.
Methods
Data of participants in the American 2017–2018 National Health and Nutrition Examination Survey were analyzed. Hepatic steatosis was defined as median controlled attenuation parameter ≥248 dB/m, which was measured by ultrasound transient elastography. MAFLD was defined by evidence of hepatic steatosis on ultrasound in addition to any metabolic dysregulation. Hepatic fibrosis was detected by FibroScan and quantified by parameter of stiffness (E). Hepatic fibrosis was defined as E ≥ 9.7 kPa. As component of CKD, reduced estimated glomerular filtration rate (eGFR) was defined as<60 mL/min/1.73 m 2 and abnormal albuminuria was defined as urinary albumin‐to‐creatinine ratio ≥ 30 mg/g.
Results
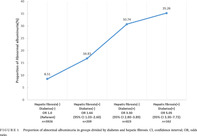
Data pertaining to 5119 participants were included in the analysis, with 40.6% hepatic normal, 52.1% MAFLD, and 7.2% hepatic fibrosis. Multivariable regression analyses showed that for abnormal albuminuria, the odds ratio (OR) was 0.82 (0.65–1.04) for MAFLD group and 1.73 (1.14.–,2.63) for hepatic fibrosis group, both taking the hepatic healthy group as reference. As for reduced eGFR, the OR was 0.68 (0.51–0.92) for MAFLD group and 0.93 (0.56–1.53) for hepatic fibrosis group. Diabetes was significantly related to greater risk of abnormal albuminuria (3.04 [2.70–3.42]) and reduced eGFR (1.53 [1.33–1.77]). With regard to the prevalence of abnormal albuminuria, the OR was 1.64 (1.03–2.60) for those with hepatic fibrosis only, 3.30 (2.80–3.89) for those with diabetes only, and 5.05 (3.30–7.72) for those with both two conditions. But there were neither additive interaction (relative excess risk due to interaction 0.56 [−1.41–.53], p = .577) nor multiplicative interaction (OR 0.81 [0.45–1.47], p = .492) between hepatic fibrosis and diabetes on the prevalence of abnormal albuminuria.
Abstract
Highlights
-
Data of 5119 participants from the American 2017–2018 National Health and Nutrition Examination Survey were analyzed.
-
In our study, hepatic steatosis was measured by ultrasound transient elastography and hepatic fibrosis was detected by FibroScan.
-
It was revealed that metabolic associated fatty liver disease (MAFLD) with hepatic fibrosis is an independent risk factor for abnormal albuminuria, whereas MAFLD without hepatic fibrosis is not associated with abnormal albuminuria.
-
MAFLD with or without hepatic fibrosis was not associated with CKD.
-
There were neither additive interaction nor multiplicative interaction between hepatic fibrosis and diabetes on the prevalence of abnormal albuminuria.
Related collections
Most cited references34
- Record: found
- Abstract: found
- Article: not found
A new equation to estimate glomerular filtration rate.
- Record: found
- Abstract: found
- Article: not found
A new definition for metabolic associated fatty liver disease: an international expert consensus statement
- Record: found
- Abstract: found
- Article: not found