- Record: found
- Abstract: found
- Article: found
Nutrition update in gastric cancer surgery

Read this article at
Abstract
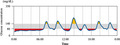
Patients with gastric cancer are often malnourished during tumor progression. Malnutrition is a risk factor for postoperative complications and a poor prognosis. Early evaluation and management of nutrition can improve these outcomes. Various combined indices in which albumin is the primary component are used to evaluate the nutritional status, including the Prognostic Nutritional Index, Glasgow Prognostic Score, and Controlling Nutritional Status score. Both the American Society for Parenteral and Enteral Nutrition and the European Society for Clinical Nutrition and Metabolism guidelines recommend immediate and early oral/enteral nutrition. However, few reports have described the additional effects of preoperative immunonutrition on clinical outcomes of gastric cancer surgery. Gastrectomy types and reconstruction methods that consider the postoperative nutritional status have been used when oncologically acceptable. Total gastrectomy has recently tended to be avoided because of its negative impact on nutritional status. New findings obtained from the emergence of continuous glucose measurement, such as glucose fluctuation and nocturnal hypoglycemia, may affect nutritional management after gastrectomy. Some prospective clinical studies on perioperative nutritional intervention have set postoperative body weight loss as a primary endpoint. It seems important to continue oral nutritional supplement, even in small doses, to reduce body weight loss after gastrectomy. Evidence generated by prospective, well‐developed randomized controlled studies must be disseminated so that nutritional therapy is widely recognized as an important multimodal therapy in patients undergoing gastric cancer surgery.
Abstract
Evaluating and addressing the issue of nutrition early can improve outcomes of gastric cancer surgery. For surgical procedures, gastrectomy types and reconstruction methods that consider postoperative nutritional status have been conducted. Evidence needs to be disseminated so that nutritional therapy is widely recognized as an important multimodal therapy for gastric cancer.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer.
- Record: found
- Abstract: not found
- Article: not found
American College of Surgeons and Surgical Infection Society: Surgical Site Infection Guidelines, 2016 Update.
- Record: found
- Abstract: found
- Article: not found