- Record: found
- Abstract: found
- Article: found
RAS Mutations Predict Recurrence-Free Survival and Recurrence Patterns in Colon Cancer: A Unicenter Study in Morocco
Read this article at
Abstract
Purpose
To date, only a few studies have investigated the role of molecular alterations in cancer recurrence. This exploratory study aimed to evaluate the impact of molecular alterations on the time and site of recurrence in patients with stage I–IV CRC and to identify the risk factors predicting recurrence-free survival in colon cancer.
Methods
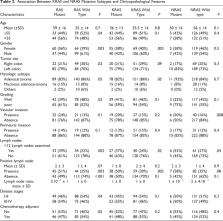
A total of 270 patients were retrospectively included. We assessed the full RAS status using Sanger and pyrosequencing. MSI status was determined by immunohistochemical analysis. Molecular alterations were correlated with recurrence timing (early or late), recurrence patterns, and recurrence-free survival. Statistical analysis was performed using the Kaplan–Meier method and the log-rank test.
Results
Of the 270 patients, 85 (31%) experienced recurrence, among whom 53% had mutant full RAS status, 48% had KRAS mutations, and 31.4% had KRAS p. G12V mutation subtype. Compared with those with late recurrence, patients with early recurrence were significantly older ( P = 0.02) and more likely to have poorly differentiated tumors, a higher rate of positive lymph nodes, KRAS mutations, and especially KRAS p. G12V mutation variant. RAS mutation status, KRAS mutations, and rare mutations are more common in patients with lung cancer recurrence. Multivariate logistic regression analysis revealed that differentiation, perineural invasion, full RAS mutation status, and KRAS codon 13 mutations were independent factors for recurrence-free survival in colon cancer.
Related collections
Most cited references41
- Record: found
- Abstract: found
- Article: not found
Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries
- Record: found
- Abstract: found
- Article: not found
The Consensus Molecular Subtypes of Colorectal Cancer
- Record: found
- Abstract: found
- Article: not found