- Record: found
- Abstract: found
- Article: found
Reconstruction of Lumbar Spinal Defects: Case Series, Literature Review, and Treatment Algorithm
Read this article at
Abstract
Background:
Lumbar spinal defects present a distinct challenge for the reconstructive surgeon and are often complicated by previous spinal surgery, the presence of hardware, and prior radiation. There are a variety of reconstructive options described but no clear treatment algorithm for these challenging defects.
Methods:
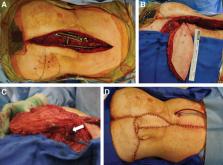
A literature search was performed to review the described treatment options for lumbar spinal soft-tissue defects. Treatments for myelomeningocele or pressure ulcers were excluded. In addition, a retrospective case review was performed for patients with lumbar defects treated with pedicled superior gluteal artery perforator (SGAP) flap reconstruction.
Results:
A literature review revealed 2,022 articles pertaining to lumbar defect reconstruction, of which 56 met inclusion criteria. These articles described 13 individual reconstructive techniques for this anatomic area. The most commonly described techniques were evaluated and a treatment algorithm designed based on patient and wound characteristics. The clinical course of 5 patients with radiated lumbar spinal defects treated with SGAP flaps is presented.
Conclusions:
There are many treatment options for lumbar spinal defects and treatment should be tailored to the patient and the characteristics of the defect. For large or radiated lumbar wounds, the pedicled SGAP flap is an excellent reconstructive choice, as it has reliable anatomy that is outside the zone of injury, adequate bulk, and minimal donor-site deficits.
Related collections
Most cited references60
- Record: found
- Abstract: found
- Article: not found
Muscle versus Fasciocutaneous Free Flaps in Lower Extremity Traumatic Reconstruction: A Multicenter Outcomes Analysis.
- Record: found
- Abstract: found
- Article: not found
Perforator-based flaps for low posterior midline defects.
- Record: found
- Abstract: found
- Article: not found