- Record: found
- Abstract: found
- Article: found
Diagnostic value of red blood cell distribution width, platelet distribution width, and red blood cell distribution width to platelet ratio in children with hemophagocytic lymphohistiocytosis
Read this article at
Abstract
Background
To investigate whether red blood cell distribution width (RDW), platelet distribution width (PDW), and red blood cell distribution width to platelet ratio (RPR) can serve as biomarkers to distinguish hemophagocytic lymphohistiocytosis (HLH) from sepsis in children.
Methods
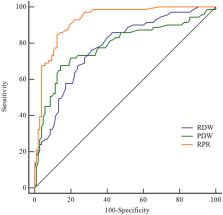
This is a retrospective study, involving 71 HLH patients, 105 sepsis patients, and 88 normal controls from January 2018 to December 2019. RDW, PDW, and RPR values were obtained from peripheral blood samples before standard treatment. The clinical differential diagnostic values of RDW, PDW, and RPR were analyzed by receiver operating characteristic (ROC) curve. In addition, peripheral blood samples after treatment from HLH patients were also collected for the same analyses.
Results
RDW, PDW, and RPR levels of the HLH patients were significantly higher than those of sepsis and normal controls ( p < 0.001). In ROC curve analysis of the RDW, PDW, and RPR for diagnosis of HLH, the area under the curve (AUC) could reach to 0.7799 (95% CI = 0.7113–0.8486), 0.7835 (95% CI = 0.7093–0.8577), and 0.9268 (95% CI = 0.8886–0.9649), respectively. When using the criteria of RDW >13.75, PDW >13.30, and RPR >0.08, the sensitivity was 76.06%, 67.61%, and 84.51%, while the specificity was 68.57%, 85.71%, and 87.62%, respectively. After treatment of HLH patients, PDW and RPR were significantly reduced ( p < 0.001).
Abstract
Comparison of laboratory parameters—RDW, PDW, and RPR among different groups. Abbreviations: RDW, red blood cell distribution width; PDW, platelet distribution width; RPR, red blood cell distribution width to platelet ratio; HLH, hemophagocytic lymphohistiocytosis. The data of PRP were shown as log 10. ** p < 0.01, *** p < 0.001.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis.
- Record: found
- Abstract: found
- Article: not found
