- Record: found
- Abstract: found
- Article: found
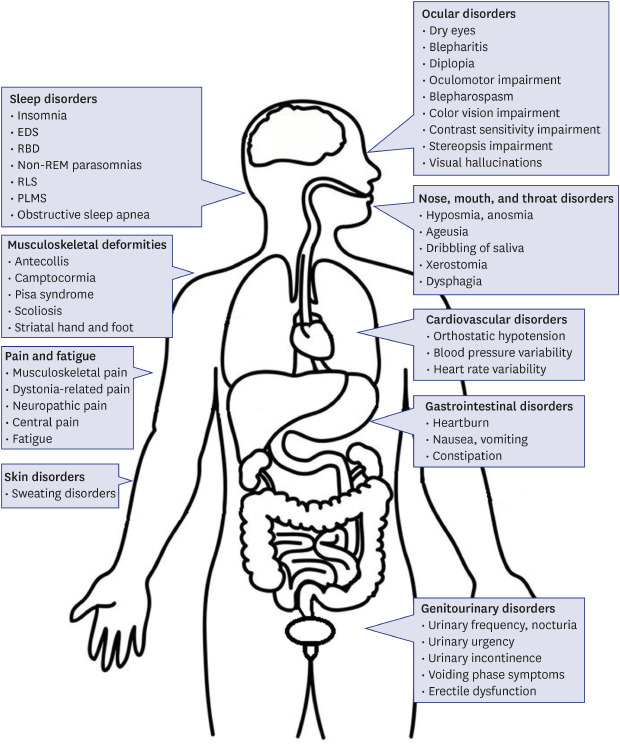
Clinical Perspectives of Parkinson's Disease for Ophthalmologists, Otorhinolaryngologists, Cardiologists, Dentists, Gastroenterologists, Urologists, Physiatrists, and Psychiatrists

Read this article at
Abstract
Parkinson's disease (PD) is a multisystemic disorder characterized by various non-motor symptoms (NMS) in addition to motor dysfunction. NMS include sleep, ocular, olfactory, throat, cardiovascular, gastrointestinal, genitourinary, or musculoskeletal disorders. A range of NMS, particularly hyposmia, sleep disturbances, constipation, and depression, can even appear prior to the motor symptoms of PD. Because NMS can affect multiple organs and result in major disabilities, the recognition and multidisciplinary and collaborative management of NMS by physicians is essential for patients with PD. Therefore, the aim of this review article is to provide an overview of the organs that are affected by NMS in PD together with a brief review of pathophysiology and treatment options.
Graphical Abstract
Related collections
Most cited references127
- Record: found
- Abstract: found
- Article: found
Update on treatments for nonmotor symptoms of Parkinson's disease—an evidence‐based medicine review
- Record: found
- Abstract: found
- Article: not found
How common is the most common adult movement disorder? Update on the worldwide prevalence of essential tremor.
- Record: found
- Abstract: found
- Article: not found