- Record: found
- Abstract: found
- Article: found
C7 slope and its association with serum lipid levels and Modic changes in patients with cervical spondylotic myelopathy
Abstract
Background: Several studies have substituted the T1 slope (T1S) with the C7 slope (C7S) because the C7 endplate is clearer on radiographs. Further, abnormal serum lipid levels have been proven to be related with the development of disc degeneration. The aim of this study was to explore the relationship between C7S, serum lipid levels, cervical parameters related to cervical sagittal balance and Modic changes (MCs) in patients with multisegment cervical spondylotic myelopathy (CSM).
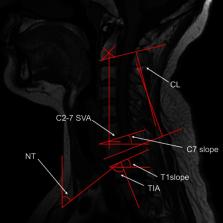
Methods: Between January 2014 and January 2017, 75 patients with multisegment CSM were enrolled in our retrospective study. Gender, age, history of smoking status and alcohol consumption, and laboratory test data were recorded. The cervical sagittal balance parameters C7S, T1S, cervical lordosis (CL), neck tilt (NT), thoracic inlet angle (TIA), C2–C7 sagittal vertical axis (SVA), and T1S-CL were analyzed with Spearman correlation tests and multiple linear regression analysis. We diagnosed MCs through computed tomography or magnetic resonance imaging of the cervical spine. Patients were divided into four subgroups according to the presence or absence of MCs and their C7S values.
Results: 75 patients were included in our study. Age, gender, C7S, and T1S were significantly different between the two groups. However, there was no statistical difference with regard to smoking status, alcohol consumption, lipoprotein(a), high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, albumin, globulin, triglycerides, total cholesterol, Ca 2+, CL, T1S, TIA, NT, and T1S−CL. The correlation between HDL-C, LDL-C, ALB, GLB, Ca 2+, C7S, T1S, MCs, NT, TIA, and C2–C7 SVA was statistically significant.
Conclusion: Significant correlations were observed between MCs and TG (as well as other preoperative sagittal parameters), which may accelerate the development of degeneration of the cervical spine. Therefore, alcohol consumption, TG, and sagittal parameters, such as C7S, and T1S could be a promising candidate for the assessment of cervical sagittal balance and predicting neck pain.
Most cited references16
- Record: found
- Abstract: not found
- Article: not found
Atherogenesis in perspective: hypercholesterolemia and inflammation as partners in crime.
- Record: found
- Abstract: found
- Article: not found