- Record: found
- Abstract: found
- Article: found
Brillouin microscopy: assessing ocular tissue biomechanics
Read this article at
Abstract
Purpose of review
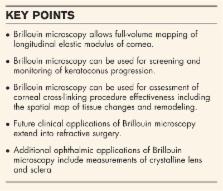
Assessment of corneal biomechanics has been an unmet clinical need in ophthalmology for many years. Many researchers and clinicians have identified corneal biomechanics as source of variability in refractive procedures and one of the main factors in keratoconus. However, it has been difficult to accurately characterize corneal biomechanics in patients. The recent development of Brillouin light scattering microscopy heightens the promise of bringing biomechanics into the clinic. The aim of this review is to overview the progress and discuss prospective applications of this new technology.
Recent findings
Brillouin microscopy uses a low-power near-infrared laser beam to determine longitudinal modulus or mechanical compressibility of tissue by analyzing the return signal spectrum. Human clinical studies have demonstrated significant difference in the elastic properties of normal corneas versus corneas diagnosed with mild and severe keratoconus. Clinical data have also shown biomechanical changes after corneal cross-linking treatment of keratoconus patients. Brillouin measurements of the crystalline lens and sclera have also been demonstrated.
Related collections
Most cited references54
- Record: found
- Abstract: found
- Article: not found
Introduction of Two Novel Stiffness Parameters and Interpretation of Air Puff-Induced Biomechanical Deformation Parameters With a Dynamic Scheimpflug Analyzer.
- Record: found
- Abstract: found
- Article: not found
Corneal biomechanical properties in normal, post-laser in situ keratomileusis, and keratoconic eyes.
- Record: found
- Abstract: found
- Article: not found