- Record: found
- Abstract: found
- Article: found
A 10 year study of hospitalized atrial fibrillation-related stroke in England and its association with uptake of oral anticoagulation
Read this article at
Abstract
Aims
To determine whether changing patterns of anticoagulant use in atrial fibrillation (AF) have impacted on stroke rates in England.
Methods and results
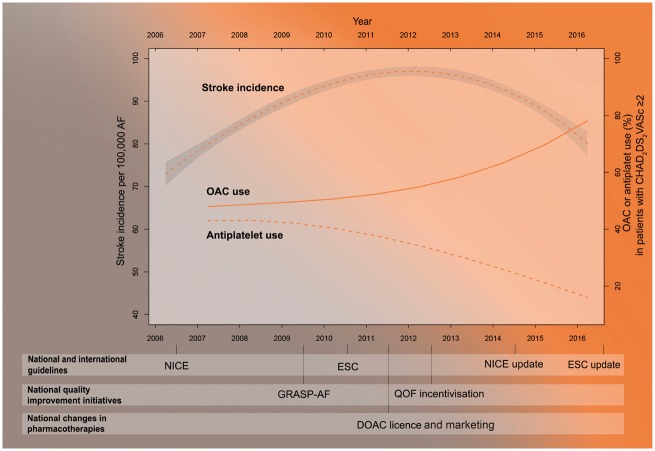
English national databases, 2006–2016, were interrogated to assess stroke admissions and oral anticoagulant use. The number of patients with known AF increased linearly from 692 054 to 983 254 (prevalence 1.29% vs. 1.71%). Hospital episodes of AF-related stroke/100 000 AF patients increased from 80/week in 2006 to 98/week in 2011 and declined to 86/week in 2016 (2006–2011 difference 18.0, 95% confidence interval (CI) 17.9–18.1, 2011–2016 difference −12.0, 95% CI −12.1 to −11.9). Anticoagulant use amongst patients with CHA 2DS 2-VASc ≥2 increased from 48.0% to 78.6% and anti-platelet use declined from 42.9% to 16.1%; the greatest rate of change occurred in the second 5 year period (for anticoagulants 2006–2011 difference 4.8%, 95% CI 4.5–5.1%, 2011–2016 difference 25.8%, 95% CI 25.5–26.1%). After adjustment for AF prevalence, a 1% increase in anticoagulant use was associated with a 0.8% decrease in the weekly rate of AF-related stroke (incidence rate ratio 0.992, 95% CI 0.989–0.994). Had the use of anticoagulants remained at 2009 levels, 4068 (95% CI 4046–4089) more strokes would have been predicted in 2015/2016.
Related collections
Most cited references10
- Record: found
- Abstract: found
- Article: not found
A multifaceted intervention to improve treatment with oral anticoagulants in atrial fibrillation (IMPACT-AF): an international, cluster-randomised trial
- Record: found
- Abstract: found
- Article: not found
Increased use of oral anticoagulants in patients with atrial fibrillation: temporal trends from 2005 to 2015 in Denmark.
- Record: found
- Abstract: found
- Article: not found