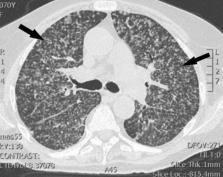
Dear Editor, We read with interest the recent article by Chen J et al., which found lower CD4+ T cells count was associated with ICU admission in patients with the coronavirus disease 2019 (COVID-19). 1 Among the clinical and laboratory features of COVID-19, a number of abnormalities have been observed and described, the most prominent of which is total lymphopenia. Through routine blood analysis, a significant reduction in lymphocytes is frequently observed; however, there still lacks thoroughly research about the lymphocyte subset counts. Here, we aimed to investigate the changes of lymphocyte subset counts in COVID-19 patients and determine if these changes are associated with disease severity and prognosis. This retrospective, single-center study was approved by the institutional ethics board of Zhongnan Hospital of Wuhan University, Wuhan, China (No. 2020015). A total of 39 RT-PCR-confirmed COVID-19 patients (admission date from January 18 to February 10, 2020) were enrolled, whose lymphocyte subset counts were tested on admission. The follow-up period lasted till Feb 19, 2020. We obtained demographic and clinical characteristics and laboratory test results from the electronic medical record system. All data were typed in a pre-designed data collection form and checked to verify data accuracy. Continuous and categorical variables were directly expressed as the median (interquartile range (IQR)) and number (%), respectively. The Mann-Whitney U test was used to compare the lymphocyte subset absolute counts of different conditions and outcomes. All statistical analyses were performed using SPSS, version 22.0 (IBM Corp., Armonk, NY). The demographic and clinical characteristics of the patients enrolled are listed in Table 1 . The median age of the patients was 53 years (IQR, 41-61), and they included 20 women and 19 men. The median of the time from onset to admission was 5 days (IQR, 3-7). On admission, leucocyte counts below the normal range appeared in 13 (34.2%) patients, and most patients had leucocyte counts within the normal range. Lymphocyte counts were below the normal range in 29 (76.3%) patients, and no patients showed an increase. The median of lymphocyte count was 0.73 × 10⁹/L (IQR, 0.56-1.07). Lymphocyte subset counts of all subsets decreased in more than half of the patients on admission. T cells decreased in 24 (61.5%) patients, CD4+ T cells decreased in 22 (56.4%) patients, CD8+ T cells decreased in 28 (71.8%) patients, B cells decreased in 27 (69.2%) patients, and NK cells decreased in 30 (76.9%) patients. No patient had subsets increased. Among patients enrolled, the median time of onset to RT-PCR turning negative was 14 (IQR, 10-20) days. Table 1 Demographic and clinical characteristics of 39 patients with COVID-19. Table 1: Characteristics (normal range) Median (IQR) / N (%) Increased, N (%) Decreased, N (%) Age, year 53 (41-61) - - Sex Female 20 (51.3) - - Male 19 (48.7) - - Onset to admission, d 5 (3-7) - - Leucocytes (3.5-9.5 × 10⁹/L) 4.11 (3.33-5.16) 13 (34.2) 3 (7.9) Lymphocytes (1.1-3.2 × 10⁹/L) 0.73 (0.56-1.07) 0 29 (76.3) T cells (805-4459 × 106/L) 561.0 (300.0-1056.0) 0 24 (61.5) CD4+ T cells (345-2350 × 106/L) 308.0 (176.0-665.0) 0 22 (56.4) CD8+ T cells (345-2350 × 106/L) 168.0 (117.0-368.0) 0 28 (71.8) CD4+/CD8+ (0.96-2.05) 1.640 (1.140-2.380) 14 (35.9) 7 (17.9) B cells (240-1317 × 106/L) 146.0 (56.0-272.0) 0 27 (69.2) NK cells (210-1514 × 106/L) 136.0 (57.0-207.0) 0 30 (76.9) Onset to RT-PCR turning negative, d 14 (10-20) - - Among the 39 patients, 15 (38.5%) had comorbidities, and 17 (43.6%) spent time from onset to admission over 5 days. According to the Guidelines for the Diagnosis and Treatment of COVID-19 (Trial Version 6), 2 21 (53.8%) patients were classified as having mild and moderate infection, 18 (46.2%) had severe and critical infection. Half of the patients (20 [51.3%]) had a negative RT-PCR result within 14 days after onset. Until the end of follow-up, 16 (43.2%) patients were given an outcome of continual cure or death. T cells, CD4+ T cells, and CD8+ T cells were all statistically higher in patients who had a mild infection, timely hospitalization, and fast recovery (all p 0.05). All analyses indicated that changes in NK cell counts and the ratio of CD4+ T cells to CD8+ T cells (CD4+/ CD8+) were not different between different conditions and outcomes. These finding are shown in Table 2 . Table 2 Lymphocyte subset counts of 39 patients with COVID-19 in different conditions and outcomes. Table 2: T cells, × 106/L CD4+ T cells, × 106/L CD8+ T cells, × 106/L CD4+ / CD8+ B cells, × 106/L NK cells, × 106/L Comorbidities No (n=24, 61.5%) 770.5 (362.0-1151.3) 476.0 (182.3-697.8) 261.0 (139.0-554.5) 1.400 (0.975-2.383) 196.5 (87.3-286.5) 147.0 (60.8-227.3) Yes (n=15, 38.5%) 375.0 (203.0-914.0) 252.0 (126.0-424.0) 142.0 (76.0-337.0) 1.870 (1.430-2.380) 91.0 (44.0-185.0) 136.0 (33.0-164.0) P value 0.069 0.133 0.046* 0.225 0.081 0.419 Onset to admission (d) ≤5 (n=22, 56.4%) 896.0 (484.5-1216.5) 530.0 (278.0-712.8) 312.5 (158.5-619.0) 1.645(1.065-2.275) 167.0 (53.5-285.3) 156.5 (45.0-254.5) >5 (n=17, 43.6%) 362.0 (258.5-605.0) 221.0 (128.0-305.5) 137.0 (88.5-205.5) 1.480 (1.160-2.490) 119.0 (69.5-232.5) 136.0 (63.0-152.0) P value 0.008* 0.017* 0.016* 0.843 0.453 0.295 Imaging changes Improvement (n=8, 25.8%) 569.5 (223.0-1020.5) 295.0 (138.5-608.5) 229.5 (81.0-354.3) 1.800 (0.960-2.180) 203.5 (59.0-286.5) 123.5 (42.0-157.8) Progression (n=23, 74.2%) 501.0 (266.0-878.0) 290.0 (148.0-630.0) 164.0 (81.0-288.0) 1.780 (1.260-2.530) 110.0 (55.0-246.0) 107.0 (31.0-192.0) P value 0.857 1.000 0.786 0.470 0.470 1.000 Severity degree Mild or moderate (n=21, 53.8%) 914.0 (468.0-1214.0) 591.0 (266.0-718.5) 288.0 (165.0-414.5) 1.780 (1.305-2.330) 174.0 (69.5-306.5) 149.0 (58.5-240.5) Severe and critical (n=18, 46.2%) 343.5(237.0-730.3) 217.5 (112.8-324.5) 122.5(76.0-256.8) 1.345 (0.930-2.413) 105.0 (55.8-235.5) 123.5(44.5-177.8) P value 0.004* 0.006* 0.011* 0.447 0.360 0.352 Oxygen therapy No (n=23, 59.0%) 896.0 (484.5-1114.0) 530.0 (278.0-679.3) 312.5 (165.5-414.3) 1.715 (1.065-2.275) 207.0 (79.8-298.8) 142.5 (58.8-217.5) Yes (n=16, 41.0%) 325.0 (223.0-605.0) 201.0 (109.5-305.5) 122.0 (74.0-191.5) 1.440 (1.200-2.445) 91.0 (55.5-190.5) 136.0 (40.0-183.0) P value 0.004* 0.013* 0.006* 0.955 0.145 0.571 Onset to RT-P CR turning negative (d) ≤14 (n=20, 51.3%) 896.0 (361.3-1156.0) 530.0 (248.3-715.0) 337.5(151.0-414.8) 1.800 (1.285-2.583) 230.5(94.3-363.0) 130.5(39.0-210.8) >14 (n=19, 48.7%) 426.0 (195.0-719.0) 242.0 (103.0-320.0) 142.0 (96.0-273.0) 1.440 (1.080-2.060) 90.0 (49.0-174.0) 136.0 (59.0-192.0) P value 0.019* 0.011* 0.046* 0.164 0.032* 1.000 Clinical outcome Hospital discharge (n=21, 56.8%) 878.0 (362.0-1256.0) 518.0 (208.0-700.0) 338.0 (154.0-511.5) 1.460 (0.980-2.335) 185.0 (72.0-282.0) 139.0 (45.5-243.5) Continual cure or death (n=16, 43.2%) 375.5 (215.0-664.5) 260.0 (129.5-317.0) 130.0 (70.0-182.0) 1.825 (1.200-2.425) 90.5 (50.5-204.3) 101.0 (51.0-160.3) P value 0.014* 0.046* 0.005* 0.399 0.098 0.350 Note: ⁎ represent the P value <0.05. Counts of lymphocyte and lymphocyte subset are of great value to ensure immune system functionality. Viral infections, immunodeficiency diseases, and other infectious diseases usually lead to abnormal changes in the levels of lymphocyte subsets. 3, 4, 5 In this study, we focused on the abnormal counts of lymphocyte and lymphocyte subset. This result is quite different from that associated with pneumonia caused by common respiratory viruses, such as respiratory syncytial virus, which is typically associated with a normal or elevated lymphocyte count. 6 Here, we found that the CD4+ T cell and CD8+ T cell counts were closely related to disease severity and clinical outcome when we compared the counts of lymphocyte subsets in different patient groups. The more serious the disease and the worse the prognosis, the lower were the T cell, CD4+ T cell, and CD8+ T cell counts on admission. Based on these findings, we believe that the CD4+ and CD8+ T cell counts in patients with COVID-9 could reflect disease severity and predict disease prognosis and are therefore good biomarkers of COVID-19 activity. In conclusion, lymphocyte subset (CD4+ and CD8+ T cell) counts reflected the disease severity and associated with clinical outcomes, which can be considered as good biomarkers of COVID-19. Early hospitalization influenced the level of CD4+ and CD8+ T cells so patients required a quick hospitalization. If patients have relatively low counts of CD4+ and CD8+ T cell on admission, they may be in a relatively severe infection with the SARS-CoV-2 virus and come to a worse prognosis. These patients should gain more attention to the change of their illness severity. Author Contributions LG and ZL contributed conception and design of the study; YH, SW, SC and MT contributed to data acquisition and check; WL performed the statistical analysis and wrote the first draft of the manuscript; WZ, LZ, MW and DC revised the tables; MW, QH, HX and WZ contributed to manuscript revision. All authors contributed to data interpretation and approved the final version. Funding sourses This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Declaration of Competing Interest None.