- Record: found
- Abstract: found
- Article: found
Recurrent embolic strokes due to antiphospholipid syndrome and non-bacterial thrombotic endocarditis in a patient with basal cell carcinoma
Read this article at
Abstract
Background
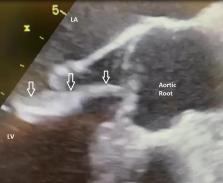
Non-Bacterial Thrombotic Endocarditis (NBTE) is a common form of aseptic thrombotic endocarditis that primarily affects mitral valves and less frequently aortic valves. NBTE is caused by systemic inflammatory reactions. This condition induces valve thickening or attached sterile mobile vegetation. NBTE is mostly asymptomatic; however, major clinical manifestations result from systemic emboli rather than valve dysfunction. When significant damage occurs, valvular insufficiency or stenosis can appear and promote heart failure occasionally requiring valve replacement surgery. NBTE is associated with hypercoagulable states, systemic lupus erythematous (SLE), antiphospholipid syndrome, or malignancies.
Case presentation
We report successful biological aortic valve replacement surgery including cardiopulmonary bypass for a 78-year-old man with NBTE and voluminous vegetation on the aortic valve inducing moderate aortic insufficiency and acute heart failure. The histopathological analysis of the valve sample showed myxoid degeneration, fibrous remodeling, and partial necrosis without any bacteria, thus indicating marantic endocarditis. Initially, the patient presented to the emergency department with an acute stroke. He was already using Apixaban treatment for a history of atrial fibrillation and cardioembolic stroke. Because of the recurrence of stroke and appearance of aortic vegetation, the investigations were extended. The antiphospholipid antibodies were positive without any indication of bacterial endocarditis. The malignancy screening was positive for basal cell carcinoma (BCC). The surgery and postoperative course were uneventful, and the patient was discharged with vitamin K antagonists (VKA). To our knowledge, NBTE with such a volume is rare and its apparent association with BCC has not been previously reported.
Conclusion
Outside of SLE and antiphospholipid syndrome, NBTE is a rare and underdiagnosed disease associated with thromboembolic events. Adequate anticoagulation is a cornerstone of its treatment. Anticoagulation management during perioperative care and valve surgery deserves specific attention and helps to protect the patient from embolic complications. In the case of stroke and thromboembolic events of unclear cause or suspected NBTE, echocardiography and thrombophilia assessments including an immunological workup are recommended.
Related collections
Most cited references25
- Record: found
- Abstract: not found
- Article: not found
2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM).
- Record: found
- Abstract: not found
- Article: not found
Diagnosis and Management of the Antiphospholipid Syndrome
- Record: found
- Abstract: not found
- Article: not found