- Record: found
- Abstract: found
- Article: found
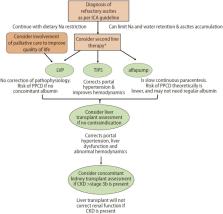
Management of refractory ascites
Read this article at
Abstract
The development of refractory ascites in approximately 10% of patients with decompensated cirrhosis heralds the progression to a more advanced stage of cirrhosis. Its pathogenesis is related to significant hemodynamic changes, initiated by portal hypertension, but ultimately leading to renal hypoperfusion and avid sodium retention. Inflammation can also contribute to the pathogenesis of refractory ascites by causing portal microthrombi, perpetuating the portal hypertension. Many complications accompany the development of refractory ascites, but renal dysfunction is most common. Management starts with continuation of sodium restriction, which needs frequent reviews for adherence; and regular large volume paracentesis of 5 L or more with albumin infusions to prevent the development of paracentesisinduced circulatory dysfunction. Albumin infusions independent of paracentesis may have a role in the management of these patients. The insertion of a covered, smaller diameter, transjugular intrahepatic porto-systemic stent shunt (TIPS) in the appropriate patients with reasonable liver reserve can bring about improvement in quality of life and improved survival after ascites clearance. Devices such as an automated low-flow ascites pump may be available in the future for ascites treatment. Patients with refractory ascites should be referred for liver transplant, as their prognosis is poor. In patients with refractory ascites and concomitant chronic kidney disease of more than stage 3b, assessment should be referred for dual liver-kidney transplants. In patients with very advanced cirrhosis not suitable for any definitive treatment for ascites control, palliative care should be involved to improve the quality of life of these patients.
Related collections
Most cited references96
- Record: found
- Abstract: not found
- Article: not found
EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis
- Record: found
- Abstract: not found
- Article: not found