- Record: found
- Abstract: found
- Article: found
Differences in artificial ligament graft osseointegration of the anterior cruciate ligament in a sheep model: a comparison between interference screw and cortical suspensory fixation
Read this article at
Abstract
Background
Interference screws are the most common femoral fixation for anterior cruciate ligament (ACL) reconstruction with polyethylene terephthalate (PET) artificial ligaments. However, interference screws have several disadvantages, such as the risk of one tunnel blowout and damage to the graft. Suspensory fixations have the advantages of high tensile strength and promotion of graft bone contact. The purpose of this study was to compare PET artificial ligament graft osseointegration between interference screw fixation (ISF) and cortical suspensory fixation (CSF) for ACL reconstruction.
Methods
Forty sheep underwent ACL reconstruction of the right knee with PET artificial ligament. The graft was fixed with ISF or CSF for femoral fixation. Animals were randomly assigned to the ISF (n=20) or the CSF (n=20) groups. The sheep were sacrificed at 3 or 12 months postoperatively for biomechanical tests, micro computed tomography (micro-CT) scans, and histological assessments.
Results
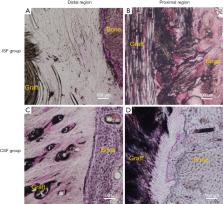
The mean load-to-failure between the CSF group (836±355 N) appeared higher than that of the ISF group (604±277 N) at 3 months, but no significant difference was detected between the groups (P=0.24). At 12 months, there was also no significant difference in load-to-failure between the CSF and ISF groups (1,194±350 vs. 1,097±764 N; P=0.78). According to the micro-CT scan results, the femoral bone tunnel diameter of the ISF group appeared larger than that of the CSF group at 3 months (12±1 vs. 10±1 mm; P=0.02) and similar to that of the CSF group at 12 months (12±1 vs. 11±2 mm; P=0.38). Furthermore, histological results showed that at the graft-tunnel interface of the femoral tunnel aperture, disoriented fibers formed in the ISF group while oriented and dense fibers formed in the CSF group.
Conclusions
ACLR with synthetic ligament by cortical suspension devices with adjustable loops demonstrated a better graft-bone healing capacity at the femoral tunnel aperture compared with that from titanium interference screws over 12 months postoperatively. No significant difference was found in biomechanical strength between the two fixation methods during the early healing stage.
Related collections
Most cited references45
- Record: found
- Abstract: found
- Article: not found
Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts.
- Record: found
- Abstract: found
- Article: not found
Bone tunnel enlargement after anterior cruciate ligament reconstruction: fact or fiction?
- Record: found
- Abstract: found
- Article: not found