- Record: found
- Abstract: found
- Article: found
Prognostic Significance of Arterial Lactate Levels at Weaning from Postcardiotomy Venoarterial Extracorporeal Membrane Oxygenation
Read this article at
Abstract
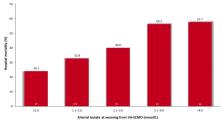
Background: The outcome after weaning from postcardiotomy venoarterial extracorporeal membrane oxygenation (VA-ECMO) is poor. In this study, we investigated the prognostic impact of arterial lactate levels at the time of weaning from postcardiotomy VA. Methods: This analysis included 338 patients from the multicenter PC-ECMO registry with available data on arterial lactate levels at weaning from VA-ECMO. Results: Arterial lactate levels at weaning from VA-ECMO (adjusted OR 1.426, 95%CI 1.157–1.758) was an independent predictor of hospital mortality, and its best cutoff values was 1.6 mmol/L (<1.6 mmol/L, 26.2% vs. ≥ 1.6 mmol/L, 45.0%; adjusted OR 2.489, 95%CI 1.374–4.505). When 261 patients with arterial lactate at VA-ECMO weaning ≤2.0 mmol/L were analyzed, a cutoff of arterial lactate of 1.4 mmol/L for prediction of hospital mortality was identified (<1.4 mmol/L, 24.2% vs. ≥1.4 mmol/L, 38.5%, p = 0.014). Among 87 propensity score-matched pairs, hospital mortality was significantly higher in patients with arterial lactate ≥1.4 mmol/L (39.1% vs. 23.0%, p = 0.029) compared to those with lower arterial lactate. Conclusions: Increased arterial lactate levels at the time of weaning from postcardiotomy VA-ECMO increases significantly the risk of hospital mortality. Arterial lactate may be useful in guiding optimal timing of VA-ECMO weaning.
Related collections
Most cited references8
- Record: found
- Abstract: found
- Article: not found
Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial.
- Record: found
- Abstract: not found
- Article: not found
Meta-Analysis of the Outcome After Postcardiotomy Venoarterial Extracorporeal Membrane Oxygenation in Adult Patients
- Record: found
- Abstract: not found
- Article: not found