- Record: found
- Abstract: found
- Article: found
Incidence and Risk Factors for Retinal Detachment Following Pediatric Cataract Surgery
Read this article at
Abstract
Background
Retinal detachment is a major postsurgical threat in pediatric cataract surgery; however, the effect of axial length remains unclear. This study aimed to assess the relationship between axial length and detachment risk in vulnerable patients.
Methods
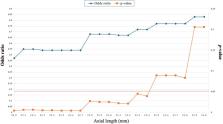
This retrospective cohort study analyzed 132 eyes of 84 pediatric cataract surgery patients aged <20 years old. Axial length was measured preoperatively, and the incidence of retinal detachment was recorded over a median follow-up of 4 years. Logistic regression analysis was used to examine the axial length-detachment relationship.
Results
Twenty eyes had postoperative retinal detachments. The median axial length was longer in the detachment group (23.6 mm) than in the non-detachment group (21.6 mm). Eyes with axial length ≤23.4 mm had 0.55-fold decreased odds of detachment compared to longer eyes. Preexisting myopia and glaucoma confer heightened risk. Approximately half of the patients retained some detachment risk eight years postoperatively.
Conclusion
Shorter eyes (axial length ≤23.4 mm) appear to be protected against pediatric retinal detachment after cataract surgery, whereas myopia, glaucoma, and axial elongation > 23.4 mm elevate the postoperative risk. Understanding these anatomical risk profiles requires surgical planning and follow-up care of children undergoing lensectomy.
Plain language Summary
This study investigated the protective role of a shorter axial length in preventing retinal detachment after pediatric cataract surgery. This highlights the correlation between smaller eye sizes and reduced detachment risk, emphasizing the need for careful consideration of anatomical factors in surgical planning and patient monitoring, particularly for patients with preexisting myopia or postoperative glaucoma.
Graphical Abstract
Related collections
Most cited references41
- Record: found
- Abstract: found
- Article: not found
The impact of ocular blood flow in glaucoma.
- Record: found
- Abstract: found
- Article: not found
Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease.
- Record: found
- Abstract: found
- Article: not found
