- Record: found
- Abstract: found
- Article: found
Outcomes of thrombolytic therapy in acute ischemic stroke: mothership, drip-and-ship, and ship-and-drip paradigms
Read this article at
Abstract
Background
Chulalongkorn Stroke Center is a comprehensive stroke center (CSC) located in Bangkok, Thailand. Our stroke network consists of different levels of spoke hospitals, ranging from community hospitals where thrombolytic treatment is not available, to those capable of onsite thrombolytic therapy. This study aimed to assess the time to treatment and outcomes among acute ischemic stroke patients who received thrombolytic treatment in the Chulalongkorn Stroke Network by 1.) Direct arrival at the CSC (mothership) 2.) Telestroke-assisted thrombolytic treatment with secondary transfer to the CSC (drip-and-ship) 3.) Referral from community hospital to the CSC for thrombolytic treatment (ship-and-drip).
Methods
Acute ischemic stroke patients who received thrombolytic treatment during January 2016–December 2017 in the Chulalongkorn Stroke Network were studied. Time to treatment and clinical outcomes were compared among treatment groups.
Results
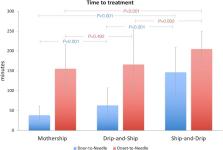
There were 273 patients in the study including 147, 87, and 39 patients in mothership, drip-and-ship, and ship-and-drip paradigms, respectively. The door-to-needle-time (DTN) and onset-to-needle-time (OTN) times were significantly longest in ship-and-drip group (146.5 ± 62/205.03 ± 44.88 mins) compared to mothership (38 ± 23/155.2 ± 60.54 mins) and drip-and-ship (63.0 ± 44/166.09 ± 87 mins), P < 0.05. There was no significant difference regarding functional independence defined by modified Rankin Scale (mRS) ≤ 2 at 3 months ( P = 0.12), in-hospital mortality ( P = 0.37), mortality at 3 months ( P = 0.73), and symptomatic intracerebral hemorrhage ( P = 0.24) among groups.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
“Telestroke”: The Application of Telemedicine for Stroke
- Record: found
- Abstract: found
- Article: not found
