- Record: found
- Abstract: found
- Article: found
Inferred duration of infectious period of SARS-CoV-2: rapid scoping review and analysis of available evidence for asymptomatic and symptomatic COVID-19 cases
Read this article at
Abstract
Objectives
Our objective was to review the literature on the inferred duration of the infectious period of COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, and provide an overview of the variation depending on the methodological approach.
Design
Rapid scoping review. Literature review with fixed search terms, up to 1 April 2020. Central tendency and variation of the parameter estimates for infectious period in (A) asymptomatic and (B) symptomatic cases from (1) virological studies (repeated testing), (2) tracing studies and (3) modelling studies were gathered. Narrative review of viral dynamics.
Information sources
Search strategies developed and the following searched: PubMed, Google Scholar, MedRxiv and BioRxiv. Additionally, the Health Information Quality Authority (Ireland) viral load synthesis was used, which screened literature from PubMed, Embase, ScienceDirect, NHS evidence, Cochrane, medRxiv and bioRxiv, and HRB open databases.
Results
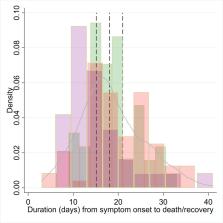
There was substantial variation in the estimates, and how infectious period was inferred. One study provided approximate median infectious period for asymptomatic cases of 6.5–9.5 days. Median presymptomatic infectious period across studies varied over <1–4 days. Estimated mean time from symptom onset to two negative RT-PCR tests was 13.4 days (95% CI 10.9 to 15.8) but was shorter when studies included children or less severe cases. Estimated mean duration from symptom onset to hospital discharge or death (potential maximal infectious period) was 18.1 days (95% CI 15.1 to 21.0); time to discharge was on average 4 days shorter than time to death. Viral dynamic data and model infectious parameters were often shorter than repeated diagnostic data.
Conclusions
There are limitations of inferring infectiousness from repeated diagnosis, viral loads and viral replication data alone and also potential patient recall bias relevant to estimating exposure and symptom onset times. Despite this, available data provide a preliminary evidence base to inform models of central tendency for key parameters and variation for exploring parameter space and sensitivity analysis.
Related collections
Most cited references83
- Record: found
- Abstract: found
- Article: not found
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China
- Record: found
- Abstract: found
- Article: not found