- Record: found
- Abstract: found
- Article: not found
Impact of Comorbidity, Race, and Marital Status in Men Referred for Prostate Biopsy with PSA >20 ng/mL: A Pilot Study in High-Risk Patients
Read this article at
Abstract
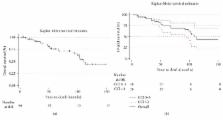
Objective. To assess the impact of comorbidity, race, and marital status on overall survival (OS) among men presenting for prostate biopsy with PSA >20 ng/mL. Methods. Data were reviewed from 2000 to 2012 and 78 patients were included in the cohort. We analyzed predictors of OS using a Cox proportional hazards model and the association between Charlson Comorbidity Index (CCI) score and PCa diagnosis or high-grade cancer using logistic regression and multinomial regression models, respectively. Results. The median age of patients was 62.5 (IQR 57–73) years. Median CCI was 3 (IQR 2–4), 69% of patients were African American men, 56% of patients were married, and 85% of patients had a positive biopsy. CCI (HR 1.52, 95% CI 1.19, 1.94), PSA (HR 1.62, 95% CI 1.09, 2.42), and Gleason sum (HR 2.04, 95% CI 1.17, 3.56) were associated with OS. CCI was associated with Gleason sum 7 (OR 4.06, 95% CI 1.04, 15.89) and Gleason sum 8–10 (OR 4.52, 95% CI 1.16, 17.54) PCa. Conclusions. CCI is an independent predictor of high-grade disease and worse OS among men with PCa. Race and marital status were not significantly associated with survival in this cohort. Patient comorbidity is an important component of determining the optimal approach to management of prostate cancer.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Bias in odds ratios by logistic regression modelling and sample size
- Record: found
- Abstract: found
- Article: not found
