- Record: found
- Abstract: found
- Article: found
Non-bacterial Thrombotic Endocarditis (NBTE) in the Absence of Malignancy or Lupus Anticoagulant/Antiphospholipid Antibodies: A Case Report
Read this article at
Abstract
Non-bacterial thrombotic endocarditis (NBTE) is a very rare condition characterized by sterile thrombi formation on cardiac valves and is often associated with hypercoagulation states, such as malignancy and autoimmune disorders.
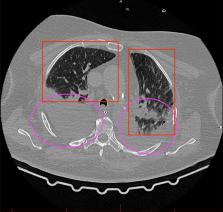
We present the case of a 74-year-old patient admitted to the intensive care unit with acute respiratory failure, who had a history of COVID-19 infection five months prior to admission, despite having received certified vaccination. The patient developed NBTE involving the mitral valve, alongside acute respiratory distress syndrome (ARDS). In spite of the exclusion of cancer and systemic connective tissue disorders, the patient's condition rapidly deteriorated, leading to treatment-resistant multi-organ failure and demise, despite aggressive management, including anticoagulation therapy, mechanical ventilation, and renal replacement therapy.
This case underscores the need for further research into the mechanisms underlying NBTE in the absence of traditional risk factors. Additionally, it highlights the importance of long-term anticoagulant therapy in NBTE management to mitigate the risk of embolic complications. Our case contributes to the growing body of literature identifying a subset of NBTE cancer-free patients with distinct characteristics, including those associated with current or past COVID-19 infection.
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: found
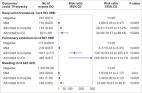
Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study
- Record: found
- Abstract: found
- Article: not found
Heart valve involvement (Libman-Sacks endocarditis) in the antiphospholipid syndrome.
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.