- Record: found
- Abstract: found
- Article: found
Using Digital Measurement–Based Care to Address Symptoms of Inattention, Hyperactivity, and Opposition in Youth: Retrospective Analysis of Bend Health
Abstract
Background
Attention-deficit/hyperactivity disorder (ADHD) and associated behavioral disorders are highly prevalent in children and adolescents, yet many of them do not receive the care they need. Digital mental health interventions (DMHIs) may address this need by providing accessible and high-quality care. Given the necessity for high levels of caregiver and primary care practitioner involvement in addressing ADHD symptoms and behavioral problems, collaborative care interventions that adopt a whole-family approach may be particularly well suited to reduce symptoms of inattention, hyperactivity, and opposition in children and adolescents.
Objective
The purpose of this study is to use member (ie, child and adolescent) data from Bend Health, Inc, a collaborative care DMHI that uses a whole-family approach to address child and adolescent mental health concerns, to (1) determine the effects of a collaborative care DMHI on inattention, hyperactivity, and oppositional symptoms in children and adolescents and (2) assess whether the effects of a collaborative care DMHI vary across ADHD subtypes and demographic factors.
Methods
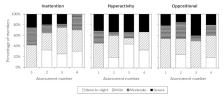
Caregivers of children and adolescents with elevated symptoms of inattention, hyperactivity, or opposition assessed their children’s symptom severity approximately every 30 days while participating in Bend Health, Inc. Data from 107 children and adolescents aged 6-17 years who exhibited clinically elevated symptoms at baseline were used to assess symptom severity across monthly assessments (inattention symptom group: n=91, 85.0%; hyperactivity symptom group: n=48, 44.9%; oppositional symptom group: n=70, 65.4%). The majority of the sample exhibited elevated symptoms of at least 2 symptom types at baseline (n=67, 62.6%).
Results
Members received care for up to 5.52 months and attended between 0 and 10 coaching, therapy, or psychiatry sessions through Bend Health, Inc. For those with at least 2 assessments, 71.0% (n=22) showed improvements in inattention symptoms, 60.0% (n=9) showed improvements in hyperactivity symptoms, and 60.0% (n=12) showed improvements in oppositional symptoms. When considering group-level change over time, symptom severity decreased over the course of treatment with Bend Health, Inc, for inattention (average decrease=3.51 points, P=.001) and hyperactivity (average decrease=3.07 points, P=.049) but not for oppositional symptoms (average decrease=0.70 points, P=.26). There was a main effect of the duration of care on symptom severity ( P<.001) such that each additional month of care was associated with lower symptom scores.
Conclusions
This study offers promising early evidence that collaborative care DHMIs may facilitate improvements in ADHD symptoms among children and adolescents, addressing the growing need for accessible and high-quality care for behavioral health problems in the United States. However, additional follow-up studies bolstered by larger samples and control groups are necessary to further establish the robustness of these findings.
Related collections
Most cited references47

- Record: found
- Abstract: found
- Article: found
Developing and Evaluating Digital Interventions to Promote Behavior Change in Health and Health Care: Recommendations Resulting From an International Workshop
- Record: found
- Abstract: found
- Article: not found