- Record: found
- Abstract: found
- Article: found
Low blood carotenoid status in dementia and mild cognitive impairment: A systematic review and meta-analysis
Read this article at
Abstract
Background
Given their potent antioxidation properties, carotenoids play a role in delaying and preventing dementia and mild cognitive impairment (MCI). However, observational studies have found inconsistent results regarding the associations between blood carotenoid levels and the risk of dementia and MCI. We conducted this systematic review and meta-analysis to investigate the relationship between blood carotenoid levels and the risk of dementia and MCI.
Methods
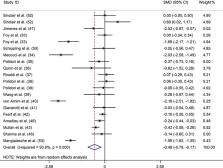
A systematic search was performed in the Web of Science, PubMed, Embase, and Cochrane Library electronic databases to retrieve relevant English articles published from their inception until February 23, 2023. Study quality was assessed by the Newcastle-Ottawa scale. Standardized mean differences (SMDs) and 95% confidence intervals (CIs) were pooled using random-effect meta-analyses. Ultimately, 23 studies (n = 6610) involving 1422 patients with dementia, 435 patients with MCI, and 4753 controls were included.
Results
Our meta-analysis showed that patients with dementia had lower blood lycopene (SMD: -0.521; 95%CI: -0.741, -0.301), α-carotene (SMD: -0.489; 95%CI: -0.697, -0.281), β-carotene (SMD: -0.476; 95%CI: -0.784, -0.168), lutein (SMD: -0.516; 95%CI: -0.753, -0.279), zeaxanthin (SMD: -0.571; 95%CI: -0.910, -0.232) and β-cryptoxanthin (SMD: -0.617; 95%CI: -0.953, -0.281) than the controls. Our results indicated that blood carotenoid levels were significantly lower in patients with dementia than in controls, despite high heterogeneity across the studies. Owing to insufficient data, we did not observe a similar and stable relationship between blood carotenoid levels and MCI.
Related collections
Most cited references56
- Record: found
- Abstract: not found
- Article: not found
Bias in meta-analysis detected by a simple, graphical test
- Record: found
- Abstract: found
- Article: not found
Quantifying heterogeneity in a meta-analysis.

- Record: found
- Abstract: found
- Article: found