- Record: found
- Abstract: found
- Article: found
Longitudinal MRI in the context of in utero surgery for open spina bifida: A descriptive study
Read this article at
Abstract
Introduction
Fetal surgery for open spina bifida (OSB) requires comprehensive preoperative assessment using imaging for appropriate patient selection and to evaluate postoperative efficacy and complications. We explored patient access and conduct of fetal magnetic resonance imaging (MRI) for prenatal assessment of OSB patients eligible for fetal surgery. We compared imaging acquisition and reporting to the International Society of Ultrasound in Obstetrics and Gynecology MRI performance guidelines.
Material and methods
We surveyed access to fetal MRI for OSB in referring fetal medicine units (FMUs) in the UK and Ireland, and two NHS England specialist commissioned fetal surgery centers (FSCs) at University College London Hospital, and University Hospitals KU Leuven Belgium. To study MRI acquisition protocols, we retrospectively analyzed fetal MRI images before and after fetal surgery for OSB.
Results
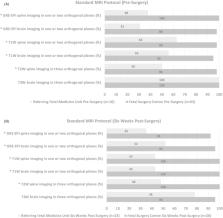
MRI for fetal OSB was accessible with appropriate specialists available to supervise, perform, and report scans. The average time to arrange a fetal MRI appointment from request was 4 ± 3 days (range, 0–10), the average scan time available was 37 ± 16 min (range, 20–80 min), with 15 ± 11 min (range, 0–30 min) extra time to repeat sequences as required. Specific MRI acquisition protocols, and MRI reporting templates were available in only 32% and 18% of units, respectively. Satisfactory T2‐weighted (T2W) brain imaging acquired in three orthogonal planes was achieved preoperatively in all centers, and 6 weeks postoperatively in 96% of FSCs and 78% of referring FMUs. However, for T2W spine image acquisition referring FMUs were less able to provide three orthogonal planes presurgery (98% FSC vs. 50% FMU, p < 0.001), and 6 weeks post‐surgery (100% FSC vs. 48% FMU, p < 0.001). Other standard imaging recommendations such as T1‐weighted (T1W), gradient echo (GE) or echoplanar fetal brain and spine imaging in one or two orthogonal planes were more likely available in FSCs compared to FMUs pre‐ and post‐surgery ( p < 0.001).
Conclusions
There was timely access to supervised MRI for OSB fetal surgery assessment. However, the provision of images of the fetal brain and spine in sufficient orthogonal planes, which are required for determining eligibility and to determine the reversal of hindbrain herniation after fetal surgery, were less frequently acquired. Our evidence suggests the need for specific guidance in relation to fetal MRI for OSB. We propose an example guidance for MRI acquisition and reporting.
Abstract
Fetal surgery for open spina bifida (OSB) is performed in selected patients. We explored ease of access, acquisition and reporting of fetal magnetic resonance imaging (MRI) in patients undergoing fetal surgery for OSB. Agreed criteria for fetal MRI in cases of OSB is a priority to ensure correct patient selection as well as to critically evaluate the efficacy of fetal surgery.
Related collections
Most cited references45
- Record: found
- Abstract: found
- Article: not found
A randomized trial of prenatal versus postnatal repair of myelomeningocele.
- Record: found
- Abstract: found
- Article: not found
Basic principles of diffusion-weighted imaging.
- Record: found
- Abstract: found
- Article: not found
