- Record: found
- Abstract: found
- Article: found
Day of week of procedure and 30 day mortality for elective surgery: retrospective analysis of hospital episode statistics
Read this article at
Abstract
Objectives To assess the association between mortality and the day of elective surgical procedure.
Design Retrospective analysis of national hospital administrative data.
Setting All acute and specialist English hospitals carrying out elective surgery over three financial years, from 2008-09 to 2010-11.
Participants Patients undergoing elective surgery in English public hospitals.
Main outcome measure Death in or out of hospital within 30 days of the procedure.
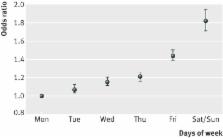
Results There were 27 582 deaths within 30 days after 4 133 346 inpatient admissions for elective operating room procedures (overall crude mortality rate 6.7 per 1000). The number of weekday and weekend procedures decreased over the three years (by 4.5% and 26.8%, respectively). The adjusted odds of death were 44% and 82% higher, respectively, if the procedures were carried out on Friday (odds ratio 1.44, 95% confidence interval 1.39 to 1.50) or a weekend (1.82, 1.71 to 1.94) compared with Monday.
Conclusions The study suggests a higher risk of death for patients who have elective surgical procedures carried out later in the working week and at the weekend.
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
Effects of weekend admission and hospital teaching status on in-hospital mortality.
- Record: found
- Abstract: found
- Article: not found
Mortality after nonemergent major surgery performed on Friday versus Monday through Wednesday.
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
