- Record: found
- Abstract: found
- Article: found
A Novel N-Arylpyridone Compound Alleviates the Inflammatory and Fibrotic Reaction of Silicosis by Inhibiting the ASK1-p38 Pathway and Regulating Macrophage Polarization
Read this article at
Abstract
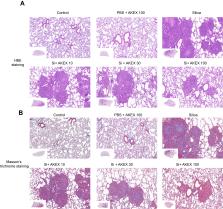
Silicosis is one of the potentially fatal occupational diseases characterized by respiratory dysfunction, chronic interstitial inflammation, and fibrosis, for which treatment options are limited. Previous studies showed that a novel N-arylpyridone compound named AKEX0011 exhibited anti-inflammatory and anti-fibrotic effects in bleomycin-induced pulmonary fibrosis; however, it is unknown whether it could also be effective against silicosis. Therefore, we sought to investigate the preventive and therapeutic roles of AKEX0011 in a silicosis rodent model and in a silica-stimulated macrophage cell line. In vivo, our results showed that AKEX0011 ameliorated silica-induced imaging lung damages, respiratory dysfunction, reduced the secretion of inflammatory and fibrotic factors (TNF-α, IL-1β, IL-6, TGF-β, IL-4, and IL-10), and the deposition of fibrosis-related proteins (collagen I, fibronectin, and α-SMA), regardless of early or advanced therapy. Specifically, we found that AKEX0011 attenuated silicosis by inhibiting apoptosis, blocking the ASK1-p38 MAPK signaling pathway, and regulating polarization of macrophages. In vitro, AKEX0011 inhibited macrophages from secreting inflammatory cytokines and inhibited apoptosis of macrophages in pre-treated and post-treated models, concurrent with blocking the ASK1-p38 pathway and inhibiting M1 polarization. Collectively, AKEX0011, as a novel N-arylpyridone compound, exerted protective effects for silica-induced pulmonary inflammation and fibrosis both in vivo and in vitro, and hence, it could be a strong drug candidate for the treatment of silicosis.
Related collections
Most cited references41
- Record: found
- Abstract: found
- Article: not found
Macrophages in Tissue Repair, Regeneration, and Fibrosis.

- Record: found
- Abstract: found
- Article: found
Molecular Mechanisms That Influence the Macrophage M1–M2 Polarization Balance
- Record: found
- Abstract: found
- Article: not found