- Record: found
- Abstract: found
- Article: found
The Comparison of the Kidney Effects of Dipeptidyl Peptidase 4 Inhibitors and Glucagon-Like Peptide 1 Agonist-Administered Concomitant with Sodium-Glucose Cotransporter 2 Inhibitors in Japanese Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease
Read this article at
Abstract
Methods
We retrospectively constructed database of 763 Japanese patients with T2DM and CKD who received sSGLT2is for more than 1 year. Among these SGLT2i-treated patients, 338 were receiving concomitant DPP4i (DPP4i group), and 99 were receiving concomitant GLP1Ra (GLP1Ra group). The two groups were compared using the propensity score matching method.
Results
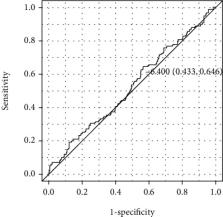
In the matched model including 86 cases per group, the decrease in the logarithmic value of the ACR and rate of reduction in the estimated glomerular filtration rate (eGFR; mL/min/1.73 m 2) of the GLP1Ra group showed no significant difference from those in the DPP4i group (−0.12 ± 0.48 vs. −0.13 ± 0.45 and −2.3 ± 18.5 vs. −6.2 ± 13.8, respectively, P = 0.10). However, the incidence of a >6.4% decrease in the eGFR was significantly lower in the GLP1Ra group than in the DPP4i group (35% vs. 52%, respectively, P = 0.03). The level of hemoglobin A 1c (mmol/mol) after SGLT2i treatment was significantly lower in the DPP4i group than in the GLP1Ra group in the matched model (58.3 ± 11.8 and 62.7 ± 14.8, respectively, P = 0.02).
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes.
- Record: found
- Abstract: found
- Article: not found
Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes
- Record: found
- Abstract: found
- Article: not found