- Record: found
- Abstract: found
- Article: found
A Review of Non-cultured Epidermal Cellular Grafting in Vitiligo
other
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
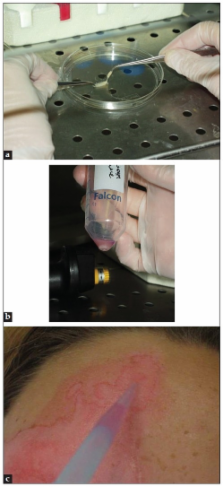
Non-cultured epidermal cellular grafting is an innovative surgical technique that can be used for the treatment of stabilized leucoderma, including vitiligo. Many reports have been published since its introduction in 1992, including several modifications and simplification of the original technique. This systematic review gives an overview of the literature.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Autologous grafting with noncultured melanocytes: a simplified method for treatment of depigmented lesions.
Y Gauthier, J E Surleve-Bazeille (1992)
- Record: found
- Abstract: found
- Article: not found
Long-term follow-up of leucoderma patients treated with transplants of autologous cultured melanocytes, ultrathin epidermal sheets and basal cell layer suspension.
Tina M. Olsson, L Juhlin (2002)
- Record: found
- Abstract: found
- Article: not found
Double-blind placebo-controlled study of autologous transplanted epidermal cell suspensions for repigmenting vitiligo.
Jean M. Naeyaert, Nanny van Geel, Katia Ongenae … (2004)