- Record: found
- Abstract: found
- Article: found
Effect of Long-Term Proton Pump Inhibitor Use on Glycemic Control in Patients with Type Two Diabetes Mellitus
Read this article at
Abstract
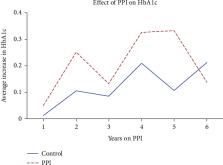
There have been conflicting results regarding the effect of proton pump inhibitors (PPIs) as an adjunctive therapy to oral antidiabetic medication (OAM) in those with type 2 diabetes (T2DM). PPIs increase gastrin levels, causing a rise in insulin. No studies have evaluated the duration of PPI therapy and its effect on glycemic control. Medical records across 8 hospitals between 2007 and 2016 were reviewed for 14,602 patients with T2DM (not on insulin therapy) taking PPIs. Values of HbA1c (baseline, follow-up, and the difference between the two) in those prescribed with PPIs and years of therapy were compared to HbA1c values of those who had no record of PPI use. Baseline and follow-up HbA1c for patients on PPIs were 6.8 and 7.0, respectively, compared to 7.1 and 7.2 in their untreated counterparts ( p < 0.001 in both comparisons). For both groups, an increase in baseline HbA1c was seen with time. Those on PPI had an increase in HbA1c of 0.16 compared to 0.08 in those not prescribed PPI. Our results show no relationship between the length of PPI therapy and HbA1c reduction.
Related collections
Most cited references12
- Record: found
- Abstract: found
- Article: not found
The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association.
- Record: found
- Abstract: found
- Article: not found
Complications of Proton Pump Inhibitor Therapy.
- Record: found
- Abstract: found
- Article: not found