- Record: found
- Abstract: found
- Article: found
Estimated glomerular filtration rate and cardiometabolic risk factors in a longitudinal cohort of children
Read this article at
Abstract
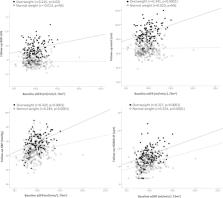
Associations between glomerular filtration rate (GFR) and cardiometabolic risk factors have been reported in adult and pediatric patients with renal disease. We aimed to assess the relationship between the estimated GFR (eGFR) and cardiometabolic risk factors in apparently healthy children. A longitudinal study in 401 asymptomatic Caucasian children (mean age 8 years) followed up after 4 years (mean age 12 years). GFR was estimated using the pediatric form of the FAS-equation. Children were classified at baseline according to their obesity status (normal weight and overweight) and according to eGFR levels (lower, average, and higher). The association of eGFR with anthropometric data [body mass index (BMI) and waist], blood pressure [systolic (SBP) and diastolic (DBP)], metabolic parameters [glucose, insulin resistance (HOMA-IR) and serum lipids], and renal ultrasonography measurements were assessed at baseline and follow-up. Baseline eGFR associated with several cardiometabolic risk factors at follow-up including higher waist, SBP, HOMA-IR, and kidney size (all p < 0.0001) in both normal weight and overweight children. In multivariate analysis, baseline eGFR was independently associated with follow-up HOMA-IR and SBP in both normal weight and overweight subjects (model R 2: 0.188–0.444), and with follow-up BMI and waist in overweight subjects (model R 2: 0.367–0.477). Moreover, children with higher filtration rates at baseline showed higher waist, SBP, DBP, HOMA-IR and renal size both at baseline and follow-up. eGFR is related to insulin resistance, blood pressure and adiposity measures in school-age children. eGFR may help to profile the cardiometabolic risk of children.
Related collections
Most cited references33

- Record: found
- Abstract: found
- Article: found
Kidney measures beyond traditional risk factors for cardiovascular prediction: A collaborative meta-analysis
- Record: found
- Abstract: found
- Article: not found
The impact of insulin resistance on the kidney and vasculature
- Record: found
- Abstract: found
- Article: not found