- Record: found
- Abstract: found
- Article: found
Serum potassium level and mineralocorticoid receptor antagonist dose in a large cohort of chronic heart failure patients
Read this article at
Abstract
Aims
Hyperkalaemia is observed frequently in heart failure (HF) patients and is associated with an impaired prognosis and underuse of mineralocorticoid receptor antagonists (MRAs). However, the effects of serum potassium on prescription of the full guideline recommended daily dose of 50 mg in real‐world daily practice are unknown. Therefore, we investigated serum potassium and its association with the prescribed MRA dose in a large cohort of chronic HF patients.
Methods and results
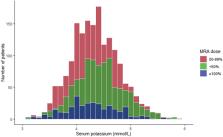
A total of 5346 patients with chronic HF with a left ventricular ejection fraction ≤40% from 34 Dutch outpatient HF clinics between 2013 and 2016 were analysed on serum potassium and MRA (spironolactone and eplenerone) dose. Data were stratified by potassium as a serum potassium level <4.0, 4.0 to 5.0 or >5.0 mmol/L. Multivariable logistic regression models were used to assess the association between serum potassium and MRA dose and to adjust for potential confounders. Mean serum potassium was 4.4 ± 0.5 mmol/L and hyperkalaemia (serum potassium >5.0 mmol/L) was present in 399 patients (7.5%). MRA was used in 3091 patients (58.1%). Patients with hyperkalaemia significantly less often received ≥100% of the target dose (50 mg) compared with patients with a serum potassium between 4.0–5.0 mmol/L and <4.0 mmol/L (7.7% vs. 9.5% vs. 13.6% respectively, P = 0.0078). In the multivariable regression analyses, patients with hyperkalaemia were significantly less likely to receive ≥100% of the target dose compared with patients with serum potassium 4.0–5.0 mmol/L (OR 0.38, 95% CI 0.15–0.97, P = 0.044). Additionally, a one unit increase in serum potassium was significantly associated with a lower odds of receiving ≥100% of the target dose (OR 0.69, 95% CI 0.49–0.98, P = 0.036).
Related collections
Most cited references34
- Record: found
- Abstract: not found
- Article: not found
2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure
- Record: found
- Abstract: found
- Article: not found
The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators.
- Record: found
- Abstract: not found
- Article: not found