- Record: found
- Abstract: found
- Article: found
Development and Validation of a Risk Stratification Model Using Disease Severity Hierarchy for Mortality or Major Cardiovascular Event
Read this article at
Key Points
Question
Does incorporating clinical domain knowledge regarding diseases, disease severity, and treatment pathways into machine learning improve risk stratification?
Findings
In this retrospective cohort study involving 51 969 patients, a new representation of patient data was developed and used to train machine learning models to predict mortality and major cardiovascular events. Results showed substantial improvement in prediction performance compared with traditional patient data representation methods.
Abstract
This cohort study introduces a new representation of patient data called disease severity hierarchy that leverages domain knowledge in a nested fashion to create subpopulations that share increasing amounts of clinical details suitable for risk prediction.
Abstract
Importance
Clinical domain knowledge about diseases and their comorbidities, severity, treatment pathways, and outcomes can facilitate diagnosis, enhance preventive strategies, and help create smart evidence-based practice guidelines.
Objective
To introduce a new representation of patient data called disease severity hierarchy that leverages domain knowledge in a nested fashion to create subpopulations that share increasing amounts of clinical details suitable for risk prediction.
Design, Setting, and Participants
This retrospective cohort study included 51 969 patients aged 45 to 85 years, with 10 674 patients who received primary care at the Mayo Clinic between January 2004 and December 2015 in the training cohort and 41 295 patients who received primary care at Fairview Health Services from January 2010 to December 2017 in the validation cohort. Data were analyzed from May 2018 to December 2019.
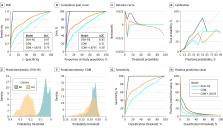
Main Outcomes and Measures
Several binary classification measures, including the area under the receiver operating characteristic curve (AUC), Gini score, sensitivity, and positive predictive value, were used to evaluate models predicting all-cause mortality and major cardiovascular events at ages 60, 65, 75, and 80 years.
Results
The mean (SD) age and proportions of women and white individuals were 59.4 (10.8) years, 6324 (59.3%) and 9804 (91.9%), respectively, in the training cohort and 57.4 (7.9) years, 21 975 (53.1%), and 37 653 (91.2%), respectively, in the validation cohort. During follow-up, 945 patients (8.9%) in the training cohort died, while 787 (7.4%) had major cardiovascular events. Models using the new representation achieved AUCs for predicting death in the training cohort at ages 60, 65, 75, and 80 years of 0.96 (95% CI, 0.94-0.97), 0.96 (95% CI, 0.95-0.98), 0.97 (95% CI, 0.96-0.98), and 0.98 (95% CI, 0.98-0.99), respectively, while standard methods achieved modest AUCs of 0.67 (95% CI, 0.55-0.80), 0.66 (95% CI, 0.56-0.79), 0.64 (95% CI, 0.57-0.71), and 0.63 (95% CI, 0.54-0.70), respectively.
Conclusions and Relevance
In this study, the proposed patient data representation accurately predicted the age at which a patient was at risk of dying or developing major cardiovascular events substantially better than standard methods. The representation uses known relationships contained in electronic health records to capture disease severity in a natural and clinically meaningful way. Furthermore, it is expressive and interpretable. This novel patient representation can help to support critical decision-making, develop smart guidelines, and enhance health care and disease management by helping to identify patients with high risk.
Related collections
Most cited references16
- Record: found
- Abstract: not found
- Article: not found
Ridge Regression: Biased Estimation for Nonorthogonal Problems
- Record: found
- Abstract: found
- Article: not found
Regularization Paths for Cox's Proportional Hazards Model via Coordinate Descent.
- Record: found
- Abstract: found
- Article: found