- Record: found
- Abstract: found
- Article: found
Multiple Shiny Papules on the Shaft of the Penis
other
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
A 26-year-old sexually active male presented to us with multiple, grouped, mildly
itchy, tiny elevated lesions on the penis for 6 months. The lesions were static since
their onset, without any increase in size and number. The patient has been married
for last 2 years and has been in a monogamous relationship since then. Before presenting
to us, the patient was treated for viral warts with topical podophyllin, but the lesions
did not resolve. Cutaneous examination revealed small, flesh-colored, shiny, papules
of around 2-3 mm in diameter on the shaft of the penis [Figure 1]. Inguinal lymph
nodes and rest of the muco-cutaneous and systemic examinations were unremarkable.
Complete hemogram and serum biochemistry panel did not reveal any abnormality. Besides,
serology for Venereal Disease Research Laboratory (VDRL) and Human Immunodeficiency
Virus (HIV) were non-reactive. The findings of histological examination of a papule
are shown in Figures 2a-b.
Figure 1
Three shiny papules on the shaft of the penis
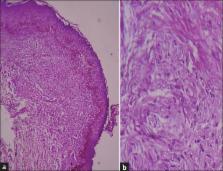
Figure 2
(a) Atrophic epidermis and proliferation of plump fibroblasts around the blood vessels
in upper dermis. (H and E ×100). (b) Higher magnification (H and E ×400)
Question
What is your diagnosis?
Answer
Ectopic pearly penile papules.
Discussion
Pearly penile papules (PPP), also known as papillomatosis corona penis, Tyson's glands,
corona capilliti, Hirsuties coronae glandis and hirsutoid papillomas, are now accepted
as normal (physiological) variation of penis and are angiofibroma histopathologically.[1]
Some authors consider these lesions as vestigial remnants of penile spines, which
are found in the same location in other primates and contributes to sexual pleasure
and quicker orgasms.[2] Vestibular papillomatosis is considered to be female equivalent
of PPP and appears as diffuse granular papules or finger-like projections that are
symmetrically distributed over the inner labia minora and vaginal introitus.[3]
PPP usually presents as one or several rows of small, flesh-colored, smooth, dome-topped
to filiform papules (1 to 3 mm in size) situated circumferentially around the corona
or sulcus of the glans penis; however, the lesions are most prominent on dorsal surface
and show a tendency to fade somewhat as they approach the frenulum.[1
2] Uncommonly, lesions may extend onto the glans penis. Lesions on the shaft of the
penis are extremely rare. Such ectopic lesions are usually associated with typical
coronal lesions, but may be the isolated finding on rare occasions.[4
5] Our case had ectopic lesions on the shaft of the penis, but he had classical PPP
lesions on corona too.
PPP are most commonly found in men between the ages of 20 and 40 years and they regress
with age.[1] However, the lesion has been described in younger patients too.[4] The
incidence of PPP reportedly ranges from 8% to 48% of male population.[6] The pathogenesis
behind their development is not clear yet. However, they are common in uncircumcised
males. In addition to this, the papules are found to regress following circumcision.[1
7] Of note, human papillomavirus (HPV) has been shown to be absent in PPP lesions.[8]
The lesions do not bear any importance in sexual activity but often, they pose a tremendous
anxiety to sexually active patients compelling them to seek medical consultations.[1]
The common clinical differentials include condyloma acuminata, molluscum contagiosum,
lichen nitidus and ectopic sebaceous glands. Histopathology is diagnostic and it reveals
thin-walled ectatic dermal blood vessels in the background of proliferation of plump
spindle-shaped stellate fibroblasts; which corroborates with a diagnosis of angiofibroma.
Elastic and reticular fibers are absent and a sparse infiltrate of mast cells, plasma
cells, lymphocytes, and histiocytes may be present in the papillary dermis. The epidermis
in PPP shows orthokeratosis, hypergranulosis, and increased size and number of epidermal
melanocytes with muted rete ridges.[9] Adenoma sebaceum (associated with tuberous
sclerosis), oral fibroma, subungual and periungual fibroma, fibrous papule of the
nose (face), and acquired acral angiofibroma are the other examples of cutaneous angiofibromas;
which have been given distinct nomenclatures based on distinctive clinical presentation
despite the fact that they share similar histopathology findings.[9
10] However, less perivascular and periadnexal fibrosis, considered another characteristic
of adenoma sebaceum, is less prominent.[10]
Masterly inactivity along with counseling regarding the benign nature of the condition
is the best treatment modality which can be offered to the patients. However, some
patients do not accept the condition and seek treatment. Options include ablative
as well as fractional lasers,[1
9
10] electrodesiccation with curettage, excisional surgery,[9
10] cryotherapy.[11] Recently, pulsed dye laser has been found to be an appropriate,
effective, and nonablative method of treatment.[12]
Related collections
Most cited references11
- Record: found
- Abstract: not found
- Article: not found
Pearly penile papules: a review.
Madhu Agrawal, Navjeevan Singh, S. Bhattacharya (2004)
- Record: found
- Abstract: found
- Article: not found
Pearly penile papules regress in older patients and with circumcision.
K. Agha, S Alderson, S Samraj … (2009)
Author and article information
Comments
Comment on this article
scite_