- Record: found
- Abstract: found
- Article: found
Extralevator abdominoperineal excision for advanced low rectal cancer: Where to go
Read this article at
Abstract
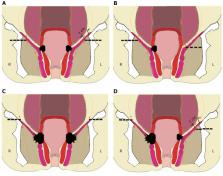
Since its introduction, extralevator abdominoperineal excision (ELAPE) in the prone position has gained significant attention and recognition as an important surgical procedure for the treatment of advanced low rectal cancer. Most studies suggest that because of adequate resection and precise anatomy, ELAPE could decrease the rate of positive circumferential resection margins, intraoperative perforation, and may further decrease local recurrence rate and improve survival. Some studies show that extensive resection of pelvic floor tissue may increase the incidence of wound complications and urogenital dysfunction. Laparoscopic/robotic ELAPE and trans-perineal minimally invasive approach allow patients to be operated in the lithotomy position, which has advantages of excellent operative view, precise dissection and reduced postoperative complications. Pelvic floor reconstruction with biological mesh could significantly reduce wound complications and the duration of hospitalization. The proposal of individualized ELAPE could further reduce the occurrence of postoperative urogenital dysfunction and chronic perianal pain. The ELAPE procedure emphasizes precise anatomy and conforms to the principle of radical resection of tumors, which is a milestone operation for the treatment of advanced low rectal cancer.
Related collections
Most cited references58
- Record: found
- Abstract: found
- Article: not found
Multicentre experience with extralevator abdominoperineal excision for low rectal cancer.
- Record: found
- Abstract: found
- Article: not found
Perineal wound healing after abdominoperineal resection for rectal cancer: a systematic review and meta-analysis.
- Record: found
- Abstract: found
- Article: not found