- Record: found
- Abstract: found
- Article: found
Comparison of Dinoprostone and Oxytocin for the Induction of Labor in Late-Term Pregnancy and the Rate of Cesarean Section: A Retrospective Study in Ten Centers in South China
Read this article at
Abstract
Background
Dinoprostone is the recommended primary option for induction of labor (IOL) in late-term pregnancies (LTPs). However, oxytocin is used in developing and rural areas, and studies have supported similar effectiveness for oxytocin and dinoprostone in reducing the rate of cesarean delivery of LTPs with a Bishop’s score of between 4–6. This study aimed to compare dinoprostone and oxytocin for IOL in LTPs and the rate of cesarean section in ten centers in South China.
Material/Methods
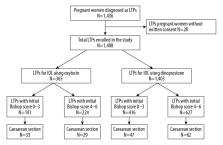
A retrospective study included 1,408 women with LTP, with subgroups including a Bishop’s score of 0–3 and 4–6. Rates of cesarean delivery were compared between women given vaginal dinoprostone and intravenous oxytocin for IOL. Secondary outcomes included the duration of labor, and maternal and fetal complications.
Results
Comparison between women who received oxytocin (N=365) and dinoprostone (N=1,043) showed significantly lower rates of cesarean delivery with dinoprostone, but no significant difference between the subgroups with Bishop’s scores of 0–3 and 4–6. The interval between induction to labor and duration of the active phase of labor were significantly reduced in the dinoprostone group with a Bishop’s score of between 4–6.
Conclusions
For LTPs with a Bishop’s score of 0–3, dinoprostone was superior to oxytocin for IOL with a lower rate of cesarean delivery, but both agents had a similar outcome for women with a Bishop’s score of 4–6. These findings may have implications for the choice of agent used in IOL when dinoprostone is unavailable.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines.
- Record: found
- Abstract: found
- Article: not found
Births: final data for 2013.
- Record: found
- Abstract: found
- Article: not found