- Record: found
- Abstract: found
- Article: found
Randomized Trial of the Effect of Mindfulness-Based Stress Reduction on Pain-Related Disability, Pain Intensity, Health-Related Quality of Life, and A1C in Patients With Painful Diabetic Peripheral Neuropathy
Read this article at
Abstract
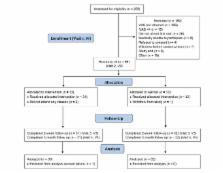
IN BRIEF Painful diabetic peripheral neuropathy (PDPN) has a large negative impact on patients’ physical and mental functioning, and pharmacological therapies rarely provide more than partial relief. Mindfulness-based stress reduction (MBSR) is a group psychosocial intervention that was developed for patients with chronic illness who were not responding to existing medical treatments. This study tested the effects of community-based MBSR courses for patients with PDPN. Among patients whose PDPN pharmacotherapy had been optimized in a chronic pain clinic, those randomly assigned to treatment with MBSR experienced improved function, better health-related quality of life, and reduced pain intensity, pain catastrophizing, and depression compared to those receiving usual care.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Neuropathic pain in the general population: a systematic review of epidemiological studies.
- Record: found
- Abstract: found
- Article: not found
Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations.
- Record: found
- Abstract: found
- Article: not found