- Record: found
- Abstract: found
- Article: found
Flash CGM Is Associated With Reduced Diabetes Events and Hospitalizations in Insulin-Treated Type 2 Diabetes
Read this article at
Abstract
Purpose
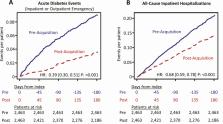
Suboptimal glycemic control among individuals with diabetes is a leading cause of hospitalizations and emergency department utilization. Use of flash continuous glucose monitoring (flash CGM) improves glycemic control in type 1 and type 2 diabetes, which may result in lower risk for acute and chronic complications that require emergency services and/or hospitalizations.
Methods
In this retrospective, real-world study, we analyzed IBM MarketScan Commercial Claims and Medicare Supplemental databases to assess the impact of flash CGM on diabetes-related events and hospitalizations in a cohort of 2463 individuals with type 2 diabetes who were on short- or rapid-acting insulin therapy. Outcomes were changes in acute diabetes-related events (ADE) and all-cause inpatient hospitalizations (ACH), occurring during the first 6 months after acquiring the flash CGM system compared with event rates during the 6 months prior to system acquisition. ICD-10 codes were used to identify ADE for hypoglycemia, hypoglycemic coma, hyperglycemia, diabetic ketoacidosis, and hyperosmolarity.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Personalized Nutrition by Prediction of Glycemic Responses.
- Record: found
- Abstract: found
- Article: not found