- Record: found
- Abstract: found
- Article: found
Trends in postpartum hemorrhage in high resource countries: a review and recommendations from the International Postpartum Hemorrhage Collaborative Group
Read this article at
Abstract
Background
Postpartum hemorrhage (PPH) is a major cause of maternal mortality and morbidity worldwide. Several recent publications have noted an increasing trend in incidence over time. The international PPH collaboration was convened to explore the observed trends and to set out actions to address the factors identified.
Methods
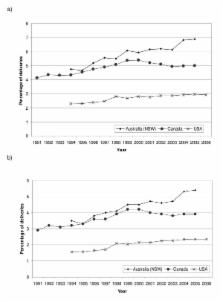
We reviewed available data sources on the incidence of PPH over time in Australia, Belgium, Canada, France, the United Kingdom and the USA. Where information was available, the incidence of PPH was stratified by cause.
Results
We observed an increasing trend in PPH, using heterogeneous definitions, in Australia, Canada, the UK and the USA. The observed increase in PPH in Australia, Canada and the USA was limited solely to immediate/atonic PPH. We noted increasing rates of severe adverse outcomes due to hemorrhage in Australia, Canada, the UK and the USA.
Conclusion
Key Recommendations
1. Future revisions of the International Classification of Diseases should include separate codes for atonic PPH and PPH immediately following childbirth that is due to other causes. Also, additional codes are required for placenta accreta/percreta/increta.
2. Definitions of PPH should be unified; further research is required to investigate how definitions are applied in practice to the coding of data.
3. Additional improvement in the collection of data concerning PPH is required, specifically including a measure of severity.
4. Further research is required to determine whether an increased rate of reported PPH is also observed in other countries, and to further investigate potential risk factors including increased duration of labor, obesity and changes in second and third stage management practice.
5. Training should be provided to all staff involved in maternity care concerning assessment of blood loss and the monitoring of women after childbirth. This is key to reducing the severity of PPH and preventing any adverse outcomes.
6. Clinicians should be more vigilant given the possibility that the frequency and severity of PPH has in fact increased. This applies particularly to small hospitals with relatively few deliveries where management protocols may not be defined adequately and drugs or equipment may not be on hand to deal with unexpected severe PPH.
Related collections
Most cited references47
- Record: found
- Abstract: found
- Article: not found
An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity.
- Record: found
- Abstract: found
- Article: not found
Prevalence and risk factors of severe obstetric haemorrhage.
- Record: found
- Abstract: found
- Article: not found