- Record: found
- Abstract: found
- Article: found
Epidemiological Pathology of Dementia: Attributable-Risks at Death in the Medical Research Council Cognitive Function and Ageing Study
Read this article at
Abstract
Researchers from the Medical Research Council Cognitive Function and Ageing Neuropathology Study carry out an analysis of brain pathologies contributing to dementia, within a cohort of elderly individuals in the UK who agreed to brain donation.
Abstract
Background
Dementia drug development aims to modulate pathological processes that cause clinical syndromes. Population data (epidemiological neuropathology) will help to model and predict the potential impact of such therapies on dementia burden in older people. Presently this can only be explored through post mortem findings. We report the attributable risks (ARs) for dementia at death for common age-related degenerative and vascular pathologies, and other factors, in the MRC Cognitive Function and Ageing Study (MRC CFAS).
Methods and Findings
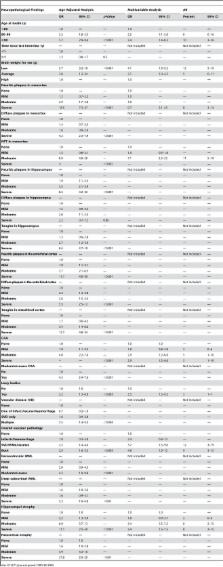
A multicentre, prospective, longitudinal study of older people in the UK was linked to a brain donation programme. Neuropathology of 456 consecutive brain donations assessed degenerative and vascular pathologies. Logistic regression modelling, with bootstrapping and sensitivity analyses, was used to estimate AR at death for dementia for specific pathologies and other factors. The main contributors to AR at death for dementia in MRC CFAS were age (18%), small brain (12%), neocortical neuritic plaques (8%) and neurofibrillary tangles (11%), small vessel disease (12%), multiple vascular pathologies (9%), and hippocampal atrophy (10%). Other significant factors include cerebral amyloid angiopathy (7%) and Lewy bodies (3%).
Conclusions
Such AR estimates cannot be derived from the living population; rather they estimate the relative contribution of specific pathologies to dementia at death. We found that multiple pathologies determine the overall burden of dementia. The impact of therapy targeted to a specific pathology may be profound when the dementia is relatively “pure,” but may be less impressive for the majority with mixed disease, and in terms of the population. These data justify a range of strategies, and combination therapies, to combat the degenerative and vascular determinants of cognitive decline and dementia.
Editors' Summary
Background
Losing one's belongings and forgetting people's names is often a normal part of aging. But increasing forgetfulness can also be a sign of dementia, a group of symptoms caused by several disorders that affect the structure of the brain. The commonest form of dementia is Alzheimer disease. In this, protein clumps called plaques and neurofibrillary tangles form in the brain and cause its degeneration. Vascular dementia, in which problems with blood circulation deprive parts of the brain of oxygen, is also common. People with dementia have problems with two or more “cognitive” functions—thinking, language, memory, understanding, and judgment. As the disease progresses, they gradually lose their ability to deal with normal daily activities until they need total care, their personality often changes, and they may become agitated or aggressive. Dementia is rare before the age of 65 years but about a quarter of people over 85 years old have dementia. Because more people live to a ripe old age these days, the number of people with dementia is increasing. According to the latest estimates, about 35 million people now have dementia and by 2050, 115 million may have the disorder.
Why Was This Study Done?
There is no cure for dementia but many drugs designed to modulate specific abnormal (pathological) changes in the brain that can cause the symptoms of dementia are being developed. To assess the likely impact of these potentially expensive new therapies, experts need to know what proportion of dementia is associated with each type of brain pathology. Although some brain changes can be detected in living brains with techniques such as computed tomography brain scans, most brain changes can only be studied in brains taken from people after death (post mortem brains). In this study, which is part of the UK Medical Research Council Cognitive Function and Ageing Study (MRC CFAS), the researchers look for associations between dementia in elderly people and pathological changes in their post mortem brains and estimate the attributable-risk (AR) for dementia at death associated with specific pathological features in the brain. That is, they estimate the proportion of dementia directly attributable to each type of pathology.
What Did the Researchers Do and Find?
Nearly 20 years ago, the MRC CFAS interviewed more than 18,000 people aged 65 years or older recruited at six sites in England and Wales to determine their cognitive function and their ability to deal with daily activities. 20% of the participants, which included people with and without cognitive impairment, were then assessed in more detail and invited to donate their brains for post mortem examination. As of 2004, 456 individuals had donated their brains. The dementia status of these donors was established using data from their assessment interviews and death certificates, and from interviews with relatives and carers, and their brains were carefully examined for abnormal changes. The researchers then used statistical methods to estimate the AR for dementia at death associated with various abnormal brain changes. The main contributors to AR for dementia at death included age (18% of dementia at death was attributable to this factor), plaques (8%), and neurofibrillary tangles (11%) in a brain region called the neocortex, small blood vessel disease (12%), and multiple abnormal changes in blood vessels (9%).
What Do These Findings Mean?
These findings suggest that multiple abnormal brain changes determine the overall burden of dementia. Importantly, they also suggest that dementia is often associated with mixed pathological changes—many people with dementia had brain changes consistent with both Alzheimer disease and vascular dementia. Because people with dementia live for variable lengths of time during which the abnormal changes in their brain are likely to alter, it may be difficult to extrapolate these findings to living populations of elderly people. Furthermore, only a small percentage of the MRC CFAS participants have donated their brains so the findings of this study may not apply to the general population. Nevertheless, these findings suggest that the new therapies currently under development may do little to reduce the overall burden of dementia because most people's dementia involves multiple pathologies. Consequently, it may be necessary to develop a range of strategies and combination therapies to deal with the ongoing dementia epidemic.
Additional Information
Please access these Web sites via the online version of this summary at http://dx.doi.org/10.1371/journal.pmed.1000180.
-
The US National Institute on Aging provides information for patients and carers about forgetfulness and about Alzheimer disease (in English and Spanish)
-
The US National Institute of Neurological Disorders and Stroke provides information about dementia (in English and Spanish)
-
The UK National Health Service Choices Web site also provides detailed information for patients and their carers about dementia and about Alzheimer disease
-
MedlinePlus provides links to additional resources about dementia and Alzheimer disease (in English and Spanish)
-
More information about the UK Medical Research Council Cognitive Function and Ageing Study (MRC CFAS) http://www.cfas.ac.ukis available
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Common structure of soluble amyloid oligomers implies common mechanism of pathogenesis.
- Record: found
- Abstract: found
- Article: not found