- Record: found
- Abstract: found
- Article: found
Nebuliser Type Influences Both Patient-Derived Bioaerosol Emissions and Ventilation Parameters during Mechanical Ventilation
Read this article at
Abstract
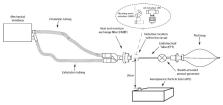
COVID-19 may lead to serious respiratory complications which may necessitate ventilatory support. There is concern surrounding potential release of patient-derived bioaerosol during nebuliser drug refill, which could impact the health of caregivers. Consequently, mesh nebulisers have been recommended by various clinical practice guidelines. Currently, there is a lack of empirical data describing the potential for release of patient-derived bioaerosol during drug refill. This study examined the release of simulated patient-derived bioaerosol, and the effect on positive end expiratory pressure during nebuliser refill during mechanical ventilation of a simulated patient. During jet nebuliser refill, the positive end expiratory pressure decreased from 4.5 to 0 cm H 2O. No loss in pressure was noted during vibrating mesh nebuliser refill. A median particle number concentration of 710 particles cm −3 above ambient was detected when refilling the jet nebuliser in comparison to no increase above ambient detected when using the vibrating mesh nebuliser. The jet nebuliser with the endotracheal tube clamped resulted in 60 particles cm −3 above ambient levels. This study confirms that choice of nebuliser impacts both the potential for patient-derived bioaerosol release and the ability to maintain ventilator circuit pressures and validates the recommended use of mesh nebulisers during mechanical ventilation.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China
- Record: found
- Abstract: found
- Article: not found
Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19)
- Record: found
- Abstract: found
- Article: not found
Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
