- Record: found
- Abstract: found
- Article: found
Five‐year survival post hepatectomy for colorectal liver metastases in a real‐world Chinese cohort: Recurrence patterns and prediction for potential cure
Read this article at
Abstract
Background
Patients with a 5‐year recurrence‐free survival post liver resection for colorectal cancer liver metastases (CRLM) are considered to be potentially cured. However, there is a deficit of data on long‐term follow‐up and the recurrence status among these patients in the Chinese population. We analyzed real‐world follow‐up data of patients with CRLM who underwent hepatectomy, explored the recurrence patterns, and established a prediction model for a potential cure scenario.
Methods
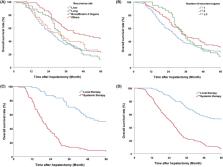
Patients who underwent radical hepatic resection for CRLM during 2000–2016, with actual follow‐up data for at least 5 years, were enrolled. The observed survival rate was calculated and compared among the groups with different recurrence patterns. The predictive factors for 5‐year non‐recurrence were determined using logistic regression analysis; a recurrence‐free survival model was developed to predict long‐term survival.
Results
A total of 433 patients were included, of whom 113 patients were found non‐recurrence after 5 years follow‐up, with a potential cure rate of 26.1%. Patients with late recurrence (>5 months) and lung relapse showed significantly superior survival. Repeated localized treatment significantly improved the long‐term survival of patients with intrahepatic or extrahepatic recurrences. Multivariate analysis showed that RAS wild‐type CRC, preoperative CEA <10 ng/ml, and liver metastases ≤3 were independent factors for a 5‐year disease‐free recurrence. A cure model was developed based on the above factors, achieving good performance in predicting long‐term survival.
Abstract
With the advances in treatment for colorectal liver metastases (CRLM), accurately predicting recurrence‐free survival post hepatectomy has become increasingly important. This study retrospectively analyzed patients with CRLM who underwent surgery with actual follow‐up over 5 years; we found that approximately one quarter of patients got a potential cure chance without recurrence. Patients with RAS wild‐type, preoperative CEA <10 ng/mL, and liver metastases ≤3 were shown to have a higher chance of cure rate after hepatic resection for CRLM.
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries
- Record: found
- Abstract: found
- Article: not found
Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases.
- Record: found
- Abstract: found
- Article: not found
