- Record: found
- Abstract: found
- Article: found
Plasma Neurofilament Light Chain and Clinical Diagnosis in Frontotemporal Dementia Syndromes
Read this article at
Abstract
Background:
Frontotemporal dementia (FTD) syndromes, mimics, phenocopy (phFTD), and slowly progressive behavioral variant FTD (bvFTD) can be difficult to distinguish clinically. Biomarkers such as neurofilament light chain (NfL) may be helpful.
Objective:
To study plasma NfL levels in people with FTD syndromes and determine if plasma NfL can distinguish between FTD syndromes and phFTD.
Methods:
Plasma NfL levels were estimated using both Simoa ® Quanterix HD-X™ and SR-X™ machines grouped via final diagnosis after investigation and review.
Results:
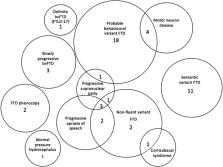
Fifty participants were studied: bvFTD = 20, semantic variant FTD (svFTD) = 11, non-fluent variant FTD (nfvFTD) = 9, FTD with motor neuron disease (MND) = 4, phFTD = 2, slow progressors = 3, FTD mimic = 1, mean age 67.2 (SD 8.4) years. NfL levels were significantly higher in the FTD group compared to phenocopy group ( p = 0.003). Median NfL (IQR) pg/mL was comparable in the FTD syndromes: bvFTD 41.10 (50.72), svFTD 44.38 (16.61), and nfvFTD 42.61 (22.93), highest in FTD with MND 79.67 (45.32) and lowest in both phFTD 13.99 (0.79) and slow progressors 17.97 (3.62).
Conclusion:
Plasma NfL appears to differentiate FTD syndromes and mimics. However, a lower NfL may predict a slower, but not necessarily absence of neurodegeneration, and therefore appears limited in distinguishing slow progressors from FTD phenocopies. Larger numbers of patients from all clinical groups are required to strengthen diagnostic utility.
Related collections
Most cited references49
- Record: found
- Abstract: found
- Article: found
Classification of primary progressive aphasia and its variants
- Record: found
- Abstract: found
- Article: found
Neurofilament light chain as a biomarker in neurological disorders
- Record: found
- Abstract: found
- Article: not found