- Record: found
- Abstract: found
- Article: found
Ambulatory Blood Pressure in Chronic Kidney Disease: Ready for Prime Time?
Read this article at
Abstract
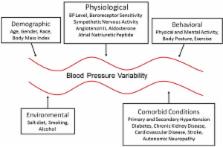
Hypertension is common in patients with chronic kidney disease (CKD) and is the most important modifiable risk factor for CKD progression and adverse cardiovascular events in these patients. Diagnosis and successful management of hypertension are critically dependent on accurate blood pressure (BP) measurement. This is most relevant to CKD patients, in whom BP control is difficult to achieve and in whom early antihypertensive treatment is imperative to prevent kidney and cardiovascular complications. Accumulated data indicate that ambulatory blood pressure monitoring (ABPM) is better in detecting hypertension than office BP measurement. ABPM is also a superior prognostic marker compared with office BP and has successfully identified hypertensive CKD patients at increased risk. Additionally, ABPM provides information on circadian BP variation and short-term BP variability, which is associated with cardiovascular and renal outcomes. This paper reviews the evidence for the usefulness of ABPM in detection and management of hypertension in CKD patients and discusses our current understanding of the pathophysiology of altered circadian BP rhythm and variability in CKD and the role of abnormal BP patterns detected by ABPM in relation to outcomes in CKD. In addition, this Review examines the emerging role of antihypertensive chronotherapy to tailor BP management to the circadian BP pattern abnormality detected by 24-hour ABPM.
Related collections
Most cited references103
- Record: found
- Abstract: found
- Article: not found
Sympathetic-nerve activity during sleep in normal subjects.
- Record: found
- Abstract: found
- Article: not found
Sympathetic overactivity in patients with chronic renal failure.
- Record: found
- Abstract: found
- Article: not found