- Record: found
- Abstract: found
- Article: found
Telehealth Utilization and Associations in the United States During the Third Year of the COVID-19 Pandemic: Population-Based Survey Study in 2022
Abstract
Background
The COVID-19 pandemic rapidly changed the landscape of clinical practice in the United States; telehealth became an essential mode of health care delivery, yet many components of telehealth use remain unknown years after the disease’s emergence.
Objective
We aim to comprehensively assess telehealth use and its associated factors in the United States.
Methods
This cross-sectional study used a nationally representative survey (Health Information National Trends Survey) administered to US adults (≥18 years) from March 2022 through November 2022. To assess telehealth adoption, perceptions of telehealth, satisfaction with telehealth, and the telehealth care purpose, we conducted weighted descriptive analyses. To identify the subpopulations with low adoption of telehealth, we developed a weighted multivariable logistic regression model.
Results
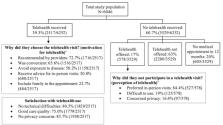
Among a total of 6252 survey participants, 39.3% (2517/6252) reported telehealth use in the past 12 months (video: 1110/6252, 17.8%; audio: 876/6252, 11.6%). The most prominent reason for not using telehealth was due to telehealth providers failing to offer this option (2200/3529, 63%). The most common reason for respondents not using offered telehealth services was a preference for in-person care (527/578, 84.4%). Primary motivations to use telehealth were providers’ recommendations (1716/2517, 72.7%) and convenience (1516/2517, 65.6%), mainly for acute minor illness (600/2397, 29.7%) and chronic condition management (583/2397, 21.4%), yet care purposes differed by age, race/ethnicity, and income. The satisfaction rate was predominately high, with no technical problems (1829/2517, 80.5%), comparable care quality to that of in-person care (1779/2517, 75%), and no privacy concerns (1958/2517, 83.7%). Younger individuals (odd ratios [ORs] 1.48-2.23; 18-64 years vs ≥75 years), women (OR 1.33, 95% CI 1.09-1.61), Hispanic individuals (OR 1.37, 95% CI 1.05-1.80; vs non-Hispanic White), those with more education (OR 1.72, 95% CI 1.03-2.87; at least a college graduate vs less than high school), unemployed individuals (OR 1.25, 95% CI 1.02-1.54), insured individuals (OR 1.83, 95% CI 1.25-2.69), or those with poor general health status (OR 1.66, 95% CI 1.30-2.13) had higher odds of using telehealth.
Conclusions
To our best knowledge, this is among the first studies to examine patient factors around telehealth use, including motivations to use, perceptions of, satisfaction with, and care purpose of telehealth, as well as sociodemographic factors associated with telehealth adoption using a nationally representative survey. The wide array of descriptive findings and identified associations will help providers and health systems understand the factors that drive patients toward or away from telehealth visits as the technology becomes more routinely available across the United States, providing future directions for telehealth use and telehealth research.
Related collections
Most cited references46
- Record: found
- Abstract: found
- Article: not found
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies.
- Record: found
- Abstract: not found
- Article: not found
Virtually Perfect? Telemedicine for Covid-19
- Record: found
- Abstract: found
- Article: not found