- Record: found
- Abstract: found
- Article: found
Uterine smooth muscle tumor of uncertain malignant potential: fertility and clinical outcomes

Read this article at
Abstract
Objective
In this study, we aimed to evaluate the clinicopathological features, obstetric, and oncological outcomes of patients diagnosed with a uterine smooth muscle tumors of uncertain malignant potential (STUMP).
Methods
A dual-institutional, database review was carried out to screen patients with STUMP who were treated with upfront surgery between January 2006 and December 2017. Data including age at the time of diagnosis, recurrence rate, disease-free survival, overall survival, and fertility outcomes were retrospectively analyzed.
Results
Fifty-seven patients with STUMPs were included in the study. The median age at the time of diagnosis was 42 (range, 16 to 75) years. The median follow-up was 57 (range, 16 to 125) months. Eight patients (14%) had recurrence during follow-up. Recurrent STUMPs were seen in seven patients and leiomyosarcoma after 14 months in one patient. Seven patients with a recurrent STUMP survived, while the remaining patient died. Recurrence rates were similar for women who underwent myomectomy and those who underwent hysterectomy. The presence of uterine localization of tumor (subserosal vs intramural-submucosal) statistically significantly affected recurrence rates (odds ratio=5.72; 95% confidence interval=1.349–24.290; p=0.018). Ten of 27 patients who underwent myomectomy for uterine myoma had fertility desire. Seven pregnancies were recorded.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Problematic uterine smooth muscle neoplasms. A clinicopathologic study of 213 cases.
- Record: found
- Abstract: found
- Article: found
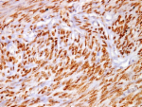
Diagnostic value of progesterone receptor and p53 expression in uterine smooth muscle tumors
- Record: found
- Abstract: found
- Article: not found