- Record: found
- Abstract: found
- Article: found
Individual and Combined Impact of Oxygen and Oxygen Transporter Supplementation during Kidney Machine Preservation in a Porcine Preclinical Kidney Transplantation Model
Read this article at
Abstract
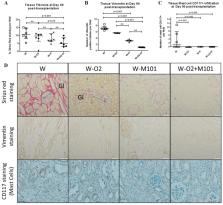
Marginal kidney graft preservation in machine perfusion (MP) is well-established. However, this method requires improvement in order to mitigate oxidative stress during ischemia-reperfusion, by using oxygenation or an O 2 carrier with anti-oxidant capacities (hemoglobin of the marine worm; M101). In our preclinical porcine (pig related) model, kidneys were submitted to 1h-warm ischemia, followed by 23 h hypothermic preservation in Waves ® MP before auto-transplantation. Four groups were studied: W (MP without 100%-O2), W-O 2 (MP with 100%-O2; also called hyperoxia), W-M101 (MP without 100%-O2 + M101 2 g/L), W-O 2 + M101 (MP with 100%-O2 + M101 2 g/L) ( n = 6/group). Results: Kidneys preserved in the W-M101 group showed lower resistance, compared to our W group. During the first week post-transplantation, W-O 2 and W-M101 groups showed a lower blood creatinine and better glomerular filtration rate. KIM-1 and IL-18 blood levels were lower in the W-M101 group, while blood levels of AST and NGAL were lower in groups with 100% O2. Three months after transplantation, fractional excretion of sodium and the proteinuria/creatinuria ratio remained higher in the W group, creatininemia was lower in the W-M101 group, and kidney fibrosis was lower in M101 groups. We concluded that supplementation with M101 associated with or without 100% O2 improved the Waves ® MP effect upon kidney recovery and late graft outcome.
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: not found
The prognostic value of renal resistance during hypothermic machine perfusion of deceased donor kidneys.
- Record: found
- Abstract: found
- Article: not found