- Record: found
- Abstract: found
- Article: found
Determinants of HIV late presentation among men who have sex with men in Portugal (2014–2019): who’s being left behind?
Read this article at
Abstract
Introduction
HIV late presentation (LP) remains excessive in Europe. We aimed to analyze the factors associated with late presentation in the MSM population newly diagnosed with HIV in Portugal between 2014 and 2019.
Methods
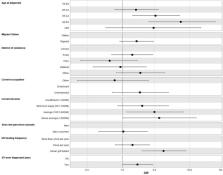
We included 391 newly HIV-1 diagnosed Men who have Sex with Men (MSM), from the BESTHOPE project, in 17 countrywide Portuguese hospitals. The data included clinical and socio-behavioral questionnaires and the viral genomic sequence obtained in the drug resistance test before starting antiretrovirals (ARVs). HIV-1 subtypes and epidemiological surveillance mutations were determined using different bioinformatics tools. Logistic regression was used to estimate the association between predictor variables and late presentation (LP).
Results
The median age was 31 years, 51% had a current income between 501–1,000 euros, 28% were migrants. 21% had never been tested for HIV before diagnosis, with 42.3% of MSM presenting LP. 60% were infected with subtype B strains. In the multivariate regression, increased age at diagnosis, higher income, lower frequency of screening, STI ever diagnosed and higher viral load were associated with LP.
Conclusion
Our study suggests that specific subgroups of the MSM population, such older MSM, with higher income and lower HIV testing frequency, are not being targeted by community and clinical screening services. Overall, targeted public health measures should be strengthened toward these subgroups, through strengthened primary care testing, expanded access to PrEP, information and promotion of HIV self-testing and more inclusive and accessible health services.
Related collections
Most cited references61
- Record: found
- Abstract: found
- Article: not found
Automated subtyping of HIV-1 genetic sequences for clinical and surveillance purposes: performance evaluation of the new REGA version 3 and seven other tools.
- Record: found
- Abstract: found
- Article: not found
Drug Resistance Mutations for Surveillance of Transmitted HIV-1 Drug-Resistance: 2009 Update
- Record: found
- Abstract: found
- Article: not found