- Record: found
- Abstract: found
- Article: found
Brain volumetric and metabolic correlates of electroconvulsive therapy for treatment-resistant depression: a longitudinal neuroimaging study
Read this article at
Abstract
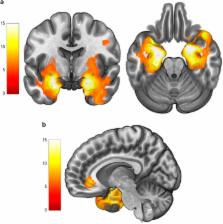
Recent research suggests that neuroplastic and neuroinflammatory changes may account for the mode of action of electroconvulsive therapy (ECT), although extant data do not allow for a clear disambiguation between these two hypotheses. Multimodal neuroimaging approaches (for example, combining structural and metabolic information) may help in clarifying this issue. Here we aimed to assess longitudinal changes in (i) regional gray matter (GM) volumes and (ii) hippocampal metabolite concentrations throughout an acute course of bitemporal ECT, as well as (iii) to determine the association between imaging changes and clinical improvement. We assessed 12 patients with treatment-resistant depression (TRD) at four time points (pre-treatment, after the first ECT session, after the ninth ECT session and 15 days after ECT course completion) and 10 healthy participants at two time points, 5 weeks apart. Patients with TRD showed bilateral medial temporal lobe (MTL) and perigenual anterior cingulate cortex volume increases. Left MTL volume increase was associated with (i) a hippocampal N-acetylaspartate concentration decrease, (ii) a hippocampal Glutamate+Glutamine concentration increase and (iii) significant clinical improvement. The observed findings are, in part, compatible with both neuroplastic and neuroinflammatory changes induced by ECT. We postulate that such phenomena may be interrelated, therefore reconciling the neuroplasticity and neuroinflammatory hypotheses of ECT action.
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: not found
Ketamine and Other NMDA Antagonists: Early Clinical Trials and Possible Mechanisms in Depression.
- Record: found
- Abstract: found
- Article: not found
Metformin activates an atypical PKC-CBP pathway to promote neurogenesis and enhance spatial memory formation.
- Record: found
- Abstract: found
- Article: not found