- Record: found
- Abstract: found
- Article: found
Efficacy of Coronary Calcium Score in Predicting Coronary Artery Morphology in Patients With Obstructive Coronary Artery Disease
Read this article at
Abstract
Background
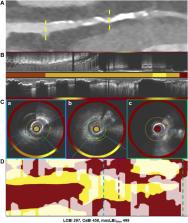
Coronary artery calcium score (CACS) is an established marker of coronary artery disease (CAD) and has been extensively used to stratify risk in asymptomatic individuals. However, the value of CACS in predicting plaque morphology in patients with advanced CAD is less established. The present analysis aims to assess the association between CACS and plaque characteristics detected by near-infrared spectroscopy-intravascular ultrasound (NIRS-IVUS) imaging in patients with obstructive CAD.
Methods
Seventy patients with obstructive CAD underwent coronary computed tomography angiography (CTA) and 3-vessel NIRS-IVUS imaging were included in the present analysis. The CTA data were used to measure the CACS in the entire coronary tree and the segments assessed by NIRS-IVUS, and these estimations were associated with the NIRS-IVUS measurements at a patient and segment level.
Results
In total, 65 patients (188 segments) completed the study protocol and were included in the analysis. A weak correlation was noted between the CACS, percent atheroma volume (r = 0.271, P = .002), and the calcific burden measured by NIRS-IVUS (r = 0.648, P < .001) at patient-level analysis. Conversely, there was no association between the CACS and the lipid content, or the incidence of high-risk plaques detected by NIRS. Linear regression analysis at the segment level demonstrated an association between the CACS and the total atheroma volume (coefficient, 0.087; 95% CI, 0.024-0.149; P = .008) and the calcific burden (coefficient, 0.117; 95% CI, 0.048-0.186; P = .001), but there was no association between the lipid content or the incidence of high-risk lesions.
Related collections
Most cited references35
- Record: found
- Abstract: not found
- Article: not found
2021 ESC Guidelines on cardiovascular disease prevention in clinical practice
- Record: found
- Abstract: found
- Article: not found
A prospective natural-history study of coronary atherosclerosis.
- Record: found
- Abstract: found
- Article: not found