- Record: found
- Abstract: found
- Article: found
A long journey for acute kidney injury biomarkers
Read this article at
Abstract
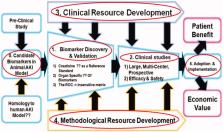
Acute kidney injury (AKI) is a life-threatening illness that continues to have an in-hospital mortality rate of patients with AKI ranges from 20% to 50% or greater, depending on underlying conditions. However, it has only marginally declined over the past 25 years. Previous authoritative publications have been pointed out that the lack of useful biomarkers for AKI has limited progress in improving the outcomes of this disorder. The purpose of this paper is to review the recent biomarkers involved in the early detection of AKI and main reasons for the failure to identify new AKI biomarkers. So far, several new AKI biomarkers have been discovered and validated to improve early diagnosis, degree of severity, pathophysiology, differential diagnosis, prediction for major kidney adverse events (MAKE, risk groups for progressive renal failure, need for renal replacement therapy [RRT], or death). These biomarkers can be classified into functional, damage and pre-injury phase biomarkers. However, the clinical use of the studied biomarkers in AKI prediction remains unclear because large prospective multicenter trials have failed to demonstrate troponin-like diagnostic performance. Reasons for the failure to identify AKI biomarkers are the heterogeneity of AKI itself, biomarker limitations and long roads to the validation of candidates for new AKI biomarkers. In an effort to overcome these barriers to identifying new AKI biomarkers, kidney biopsy specimens should be obtained and assessed in human AKI populations. Research in this field should be carried out in a pan-social approach rather than conducted by just a few medical institutions.
Related collections
Most cited references71

- Record: found
- Abstract: found
- Article: found
Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury
- Record: found
- Abstract: found
- Article: not found
Kidney injury molecule-1 (KIM-1), a putative epithelial cell adhesion molecule containing a novel immunoglobulin domain, is up-regulated in renal cells after injury.
- Record: found
- Abstract: found
- Article: not found